Troubleshooting difficult SVT ablation

Raja Selvaraj
Professor of Cardiology, JIPMER
General
- Do not ablate without making a diagnosis
- Do not ablate without mapping completely
- Do not ablate unless you are sure you can recognize and avoid AV block
- Except specific situations, high power ablation does not succeed where low power fails
- Do not ablate for cosmetic reasons
AVNRT
Left sided ablation
VA block during ablation
Accessory pathways
RF parameters to identify effective ablation

Safest ablation is the one that you avoid !
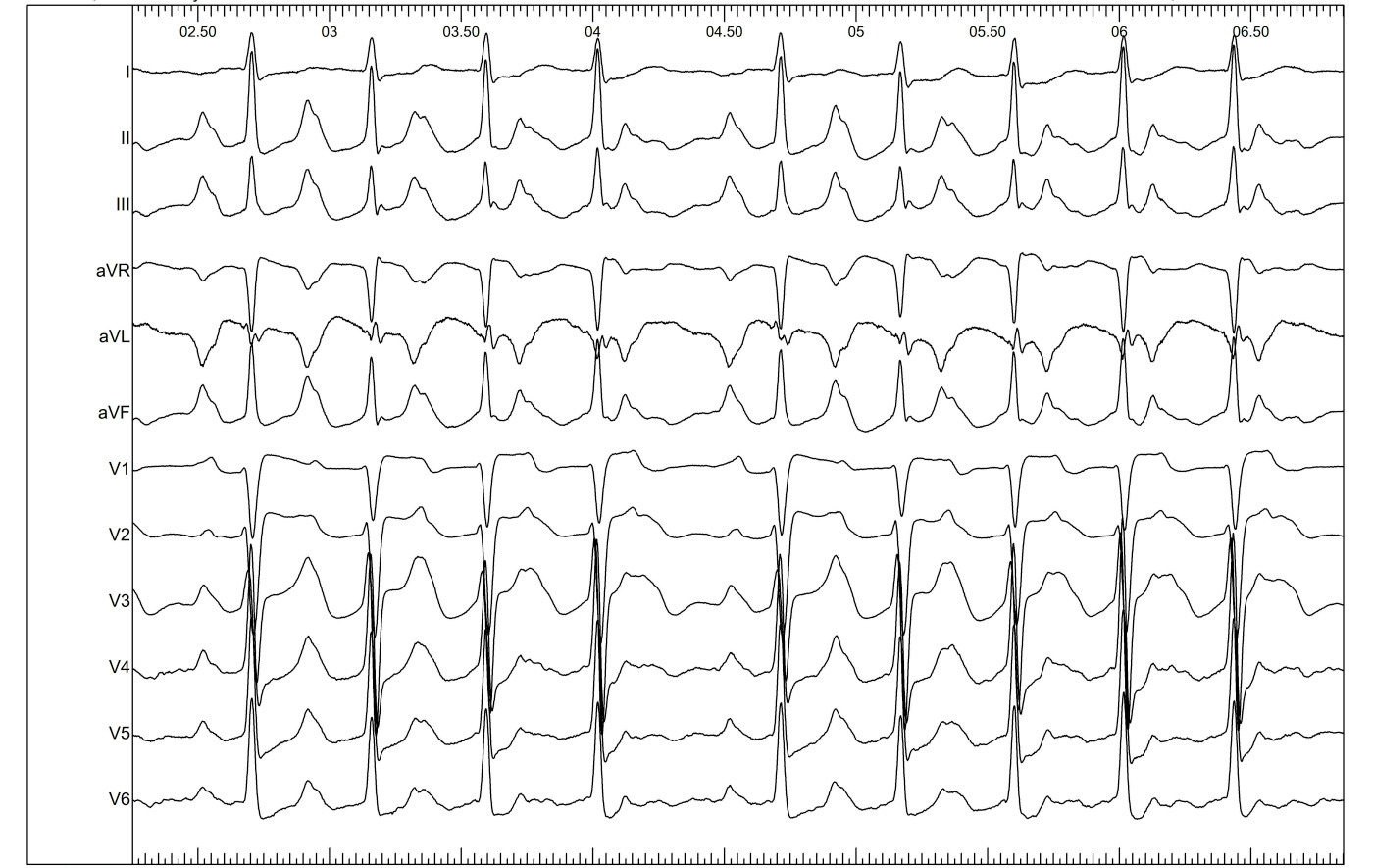
Young male. preexcitation and atypical symptoms

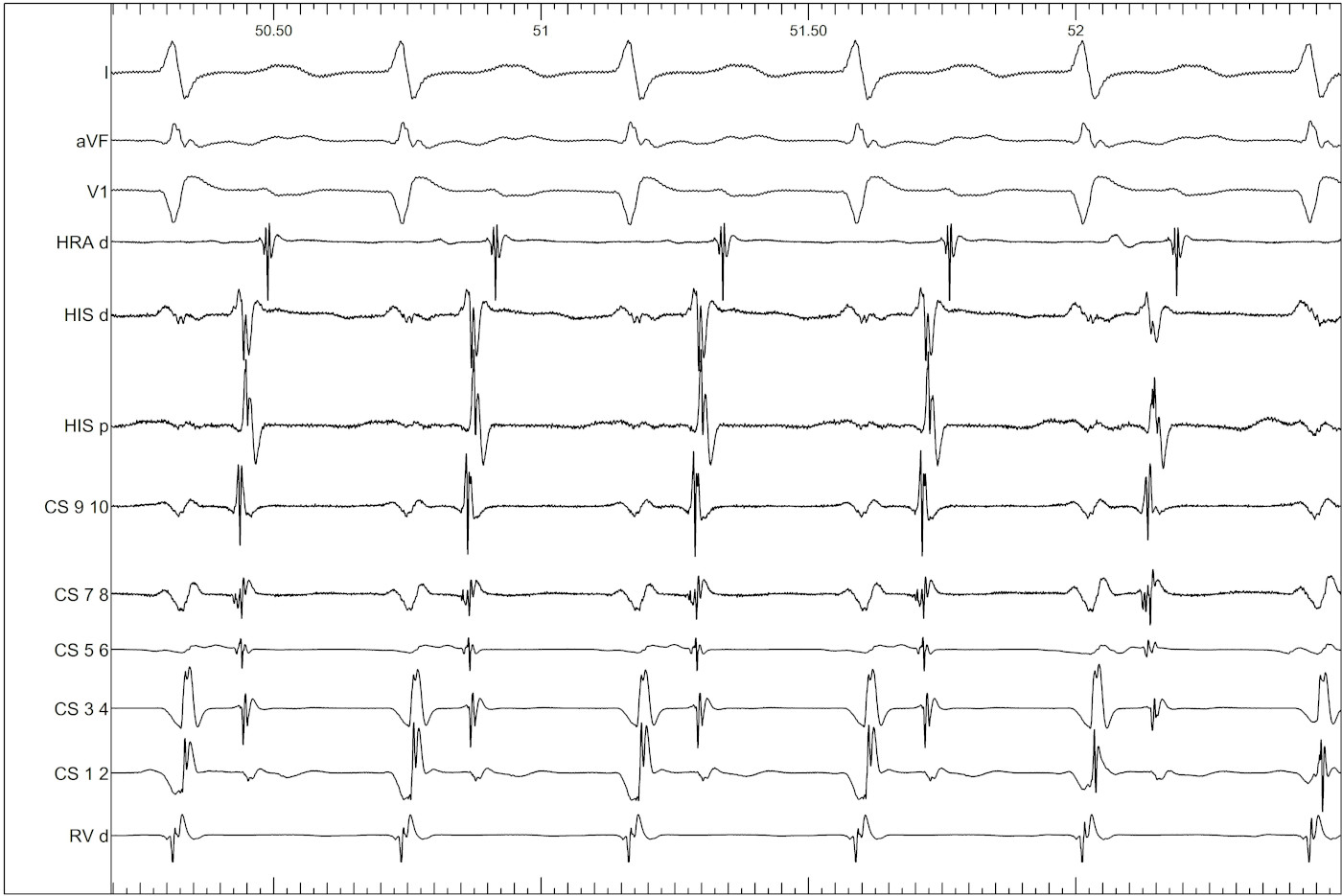
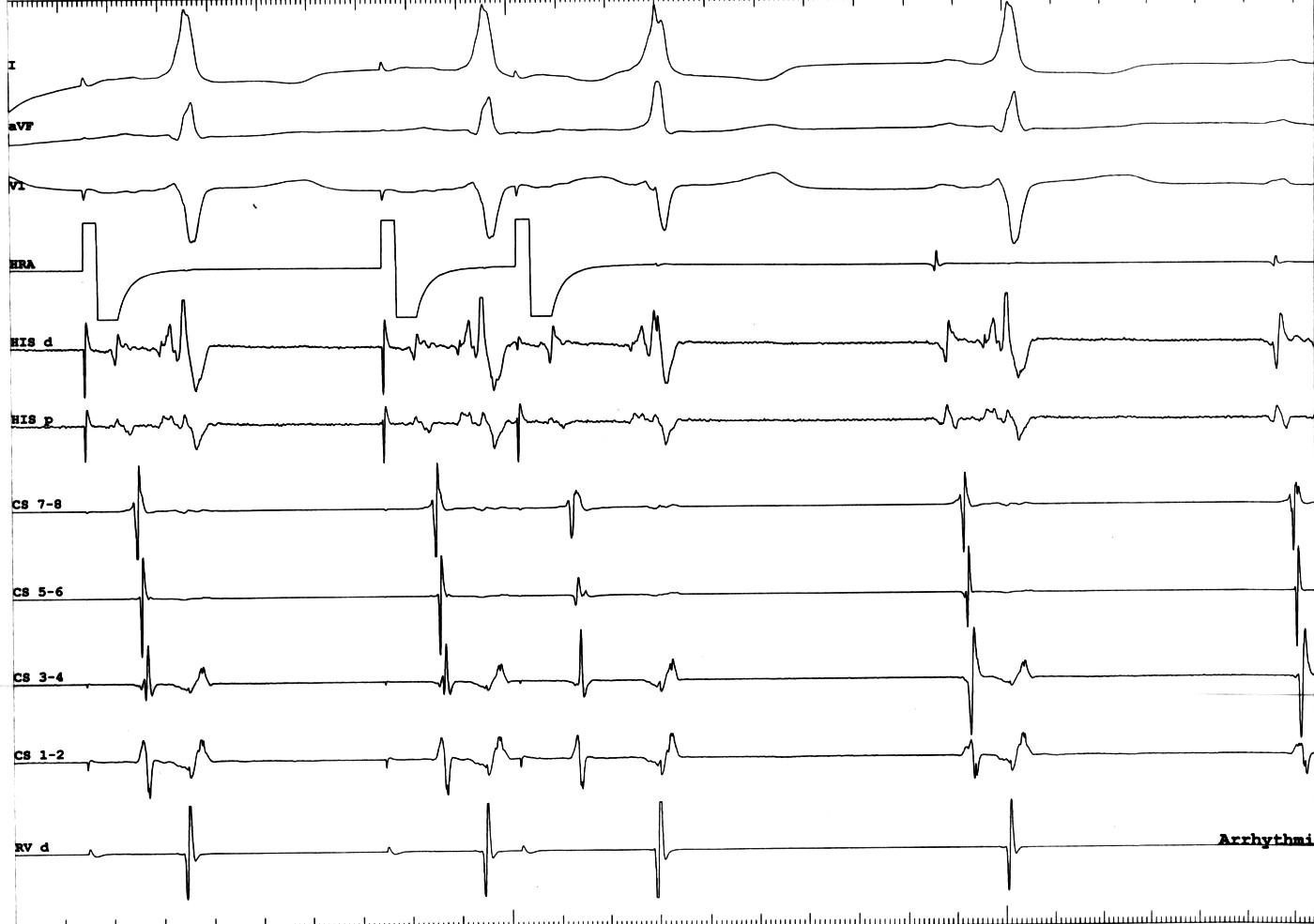
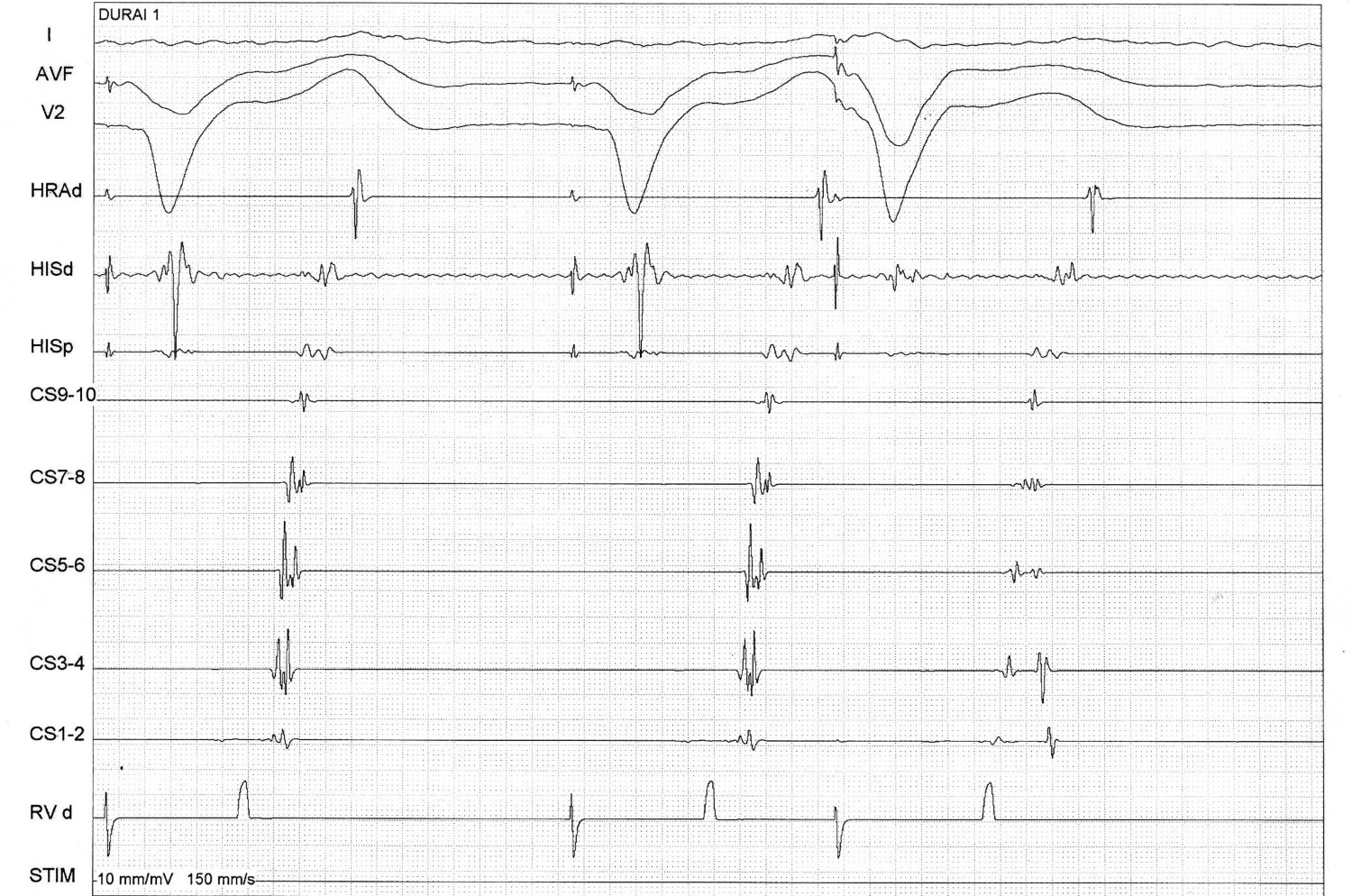
Atrial S1S2 - 600/290 ms

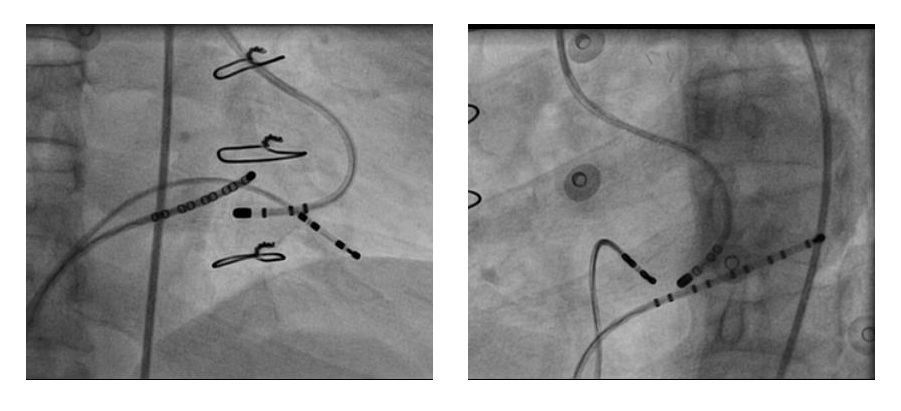
Parahisian pacing

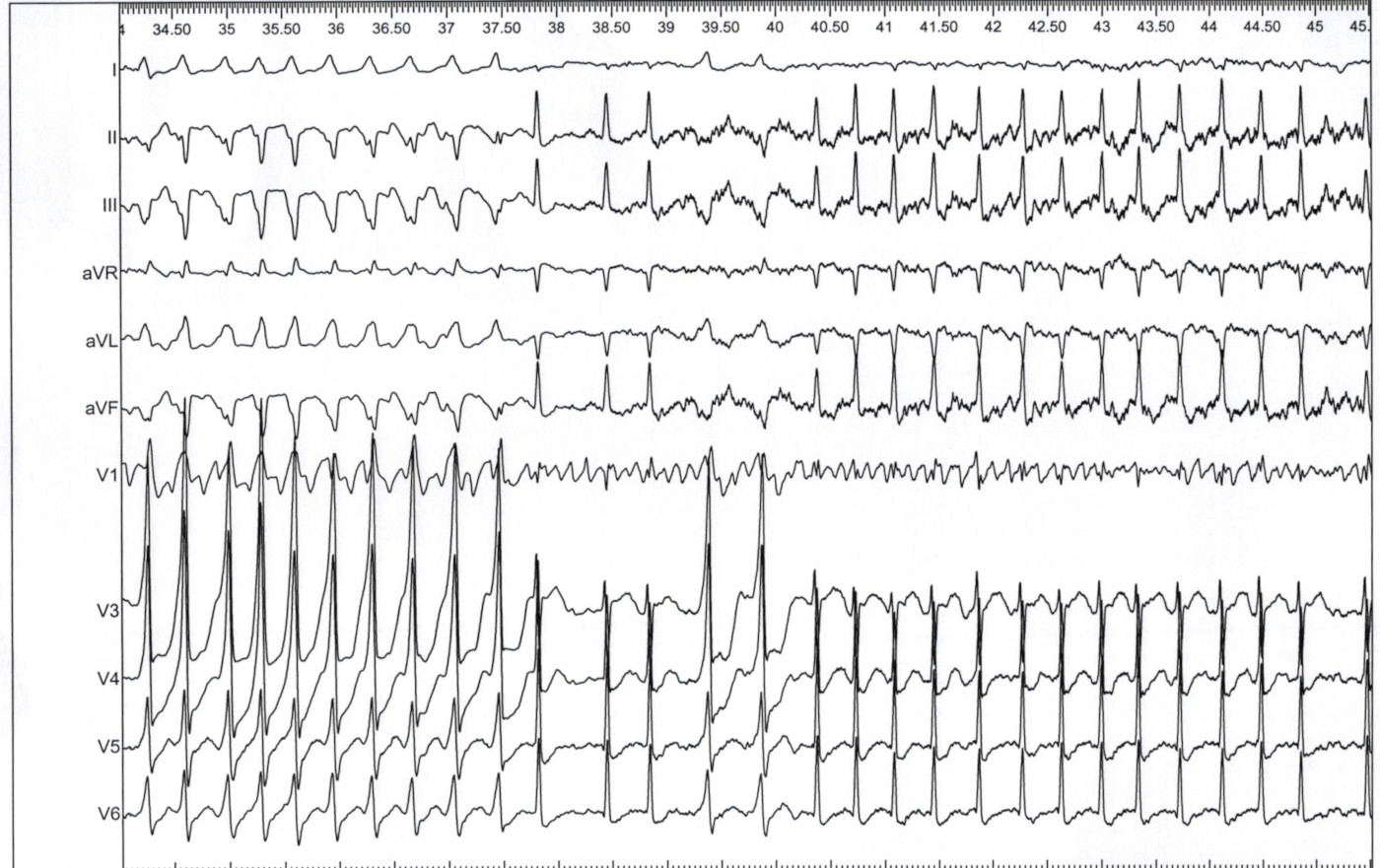
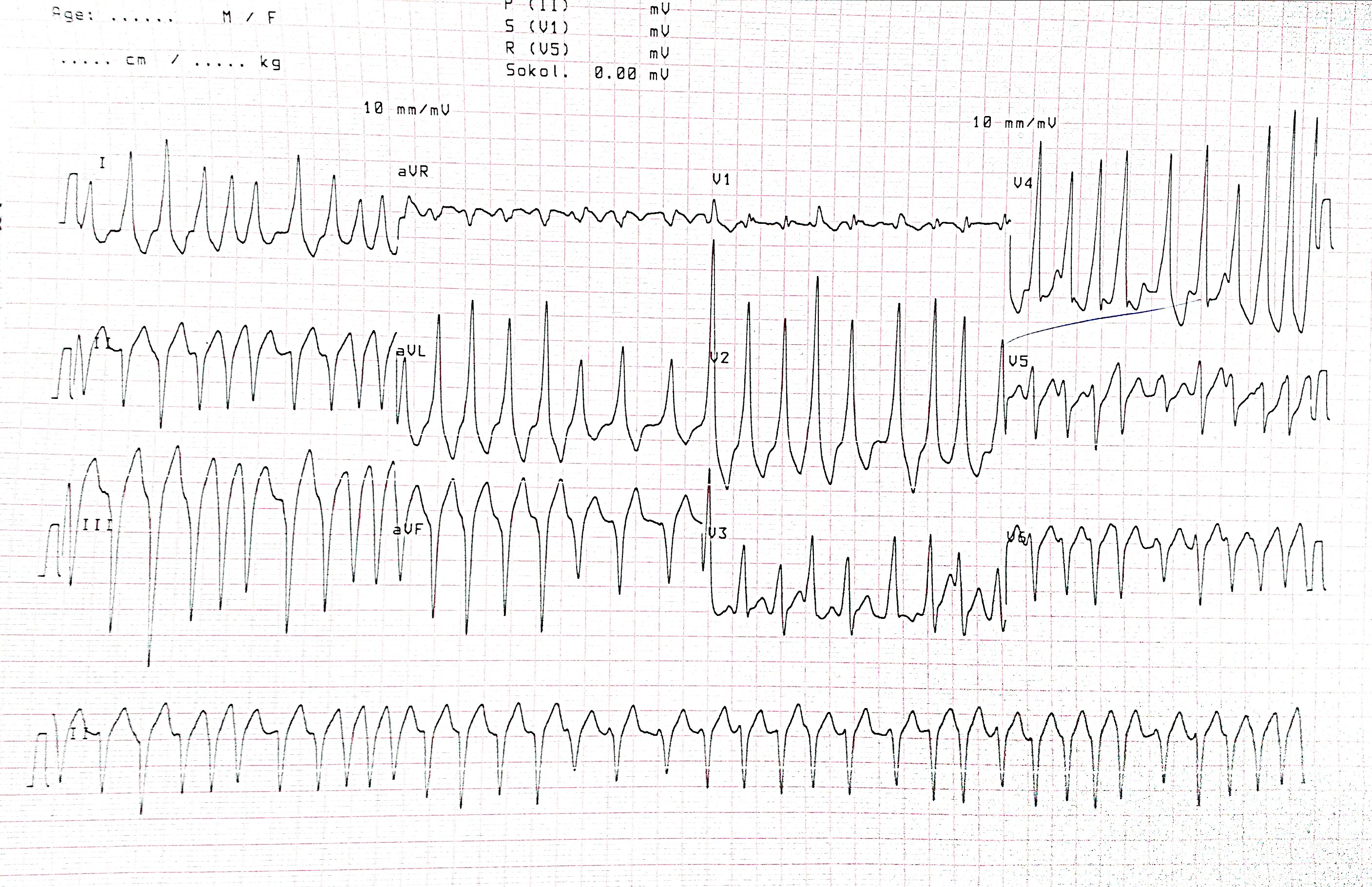
AF induced

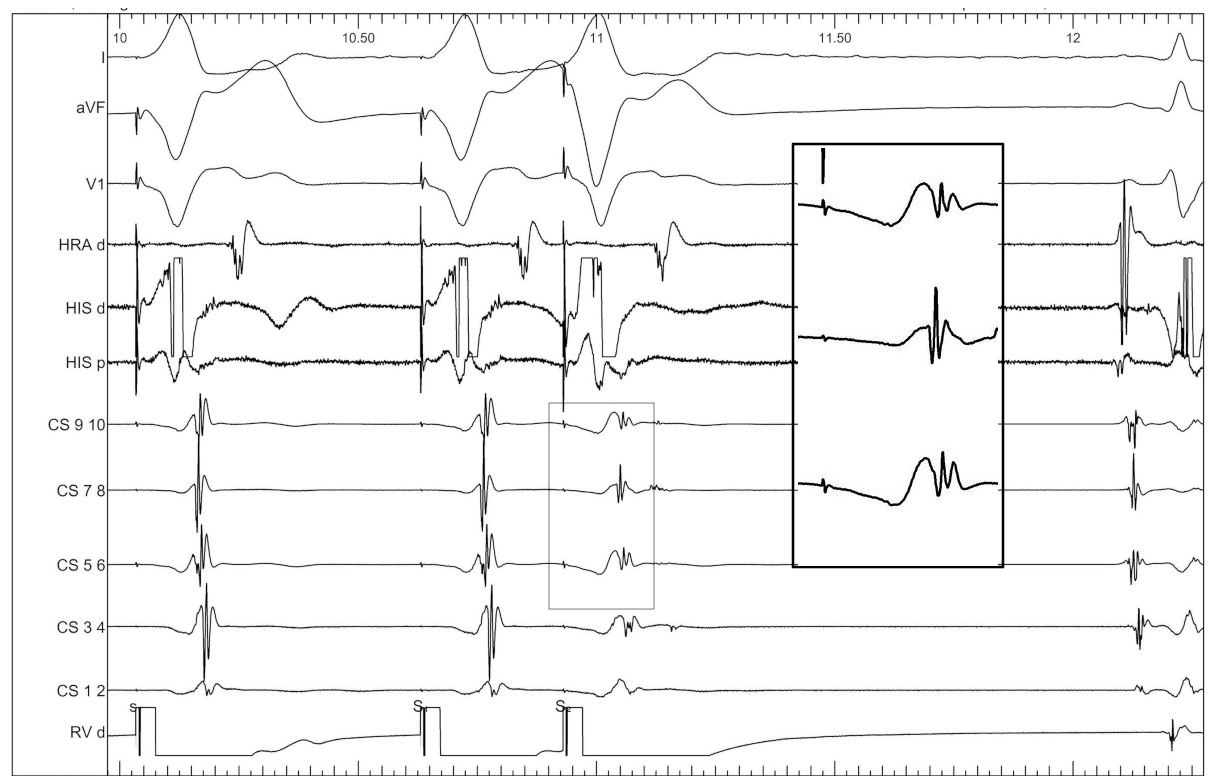
Young boy with preexcitation
Mapping approaches - Rhythm
Mapping approaches
- Earliest ventricular activation during maximum preexcitation with atrial pacing *
- Earliest atrial activation during ventricular pacing *
- Earliest atrial activation during orthodromic reentrant tachycardia
- Intermediate preexcitation during sinus rhythm / slow pacing
(*) May not recognise AV conduction injury
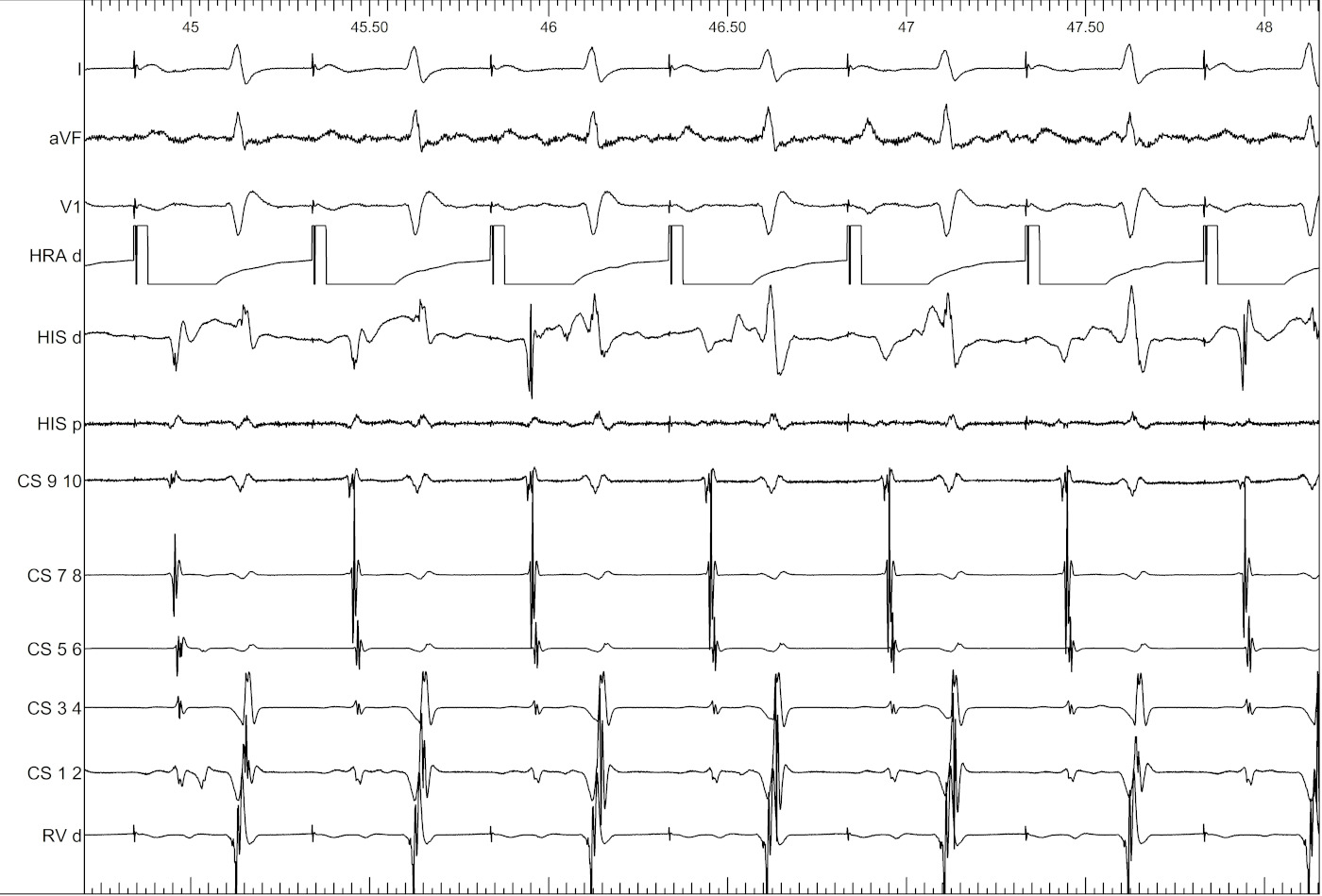
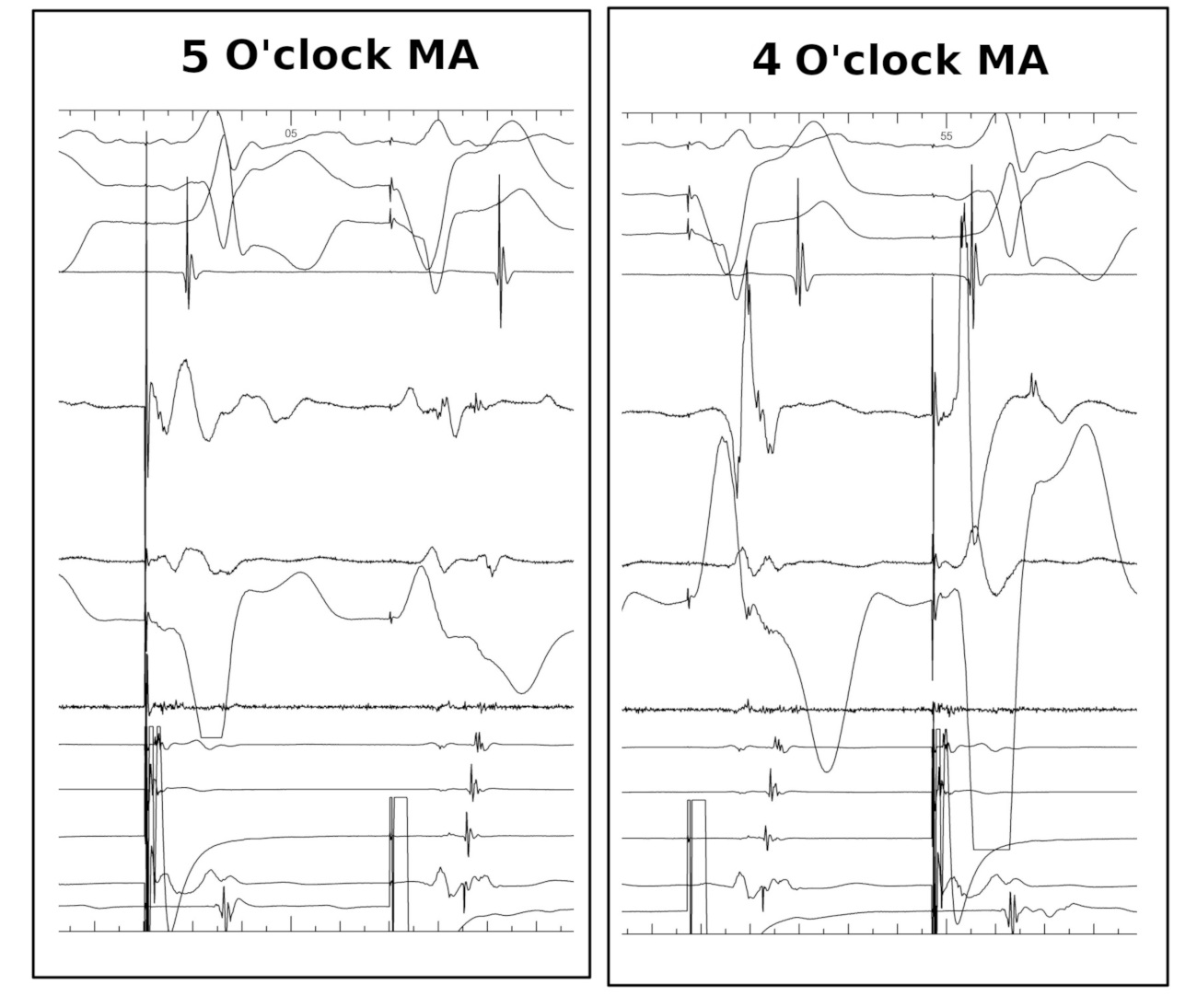
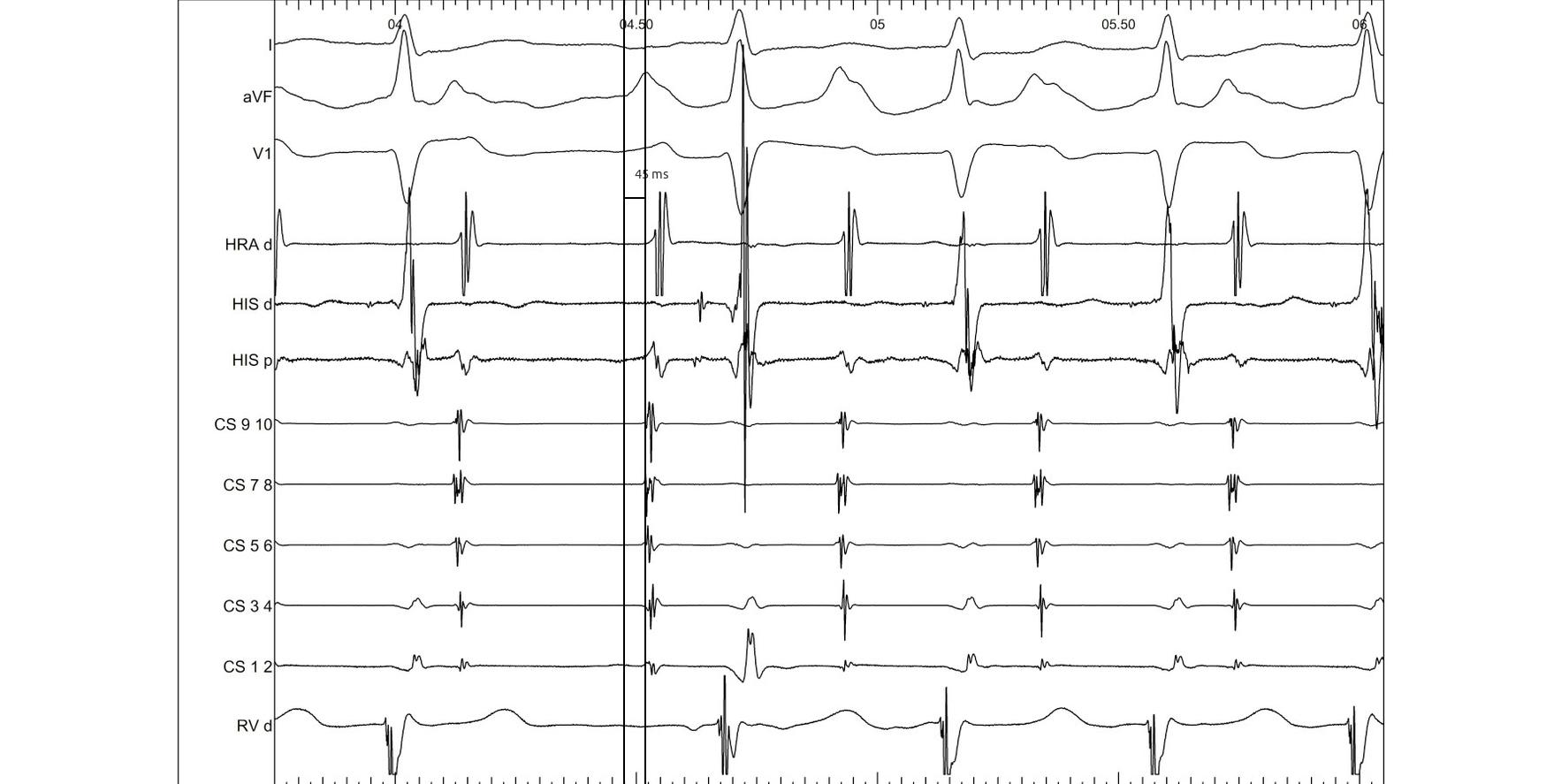
Septal pathways - Ablate during tachycardia
Left sided pathways - Entrain and ablate

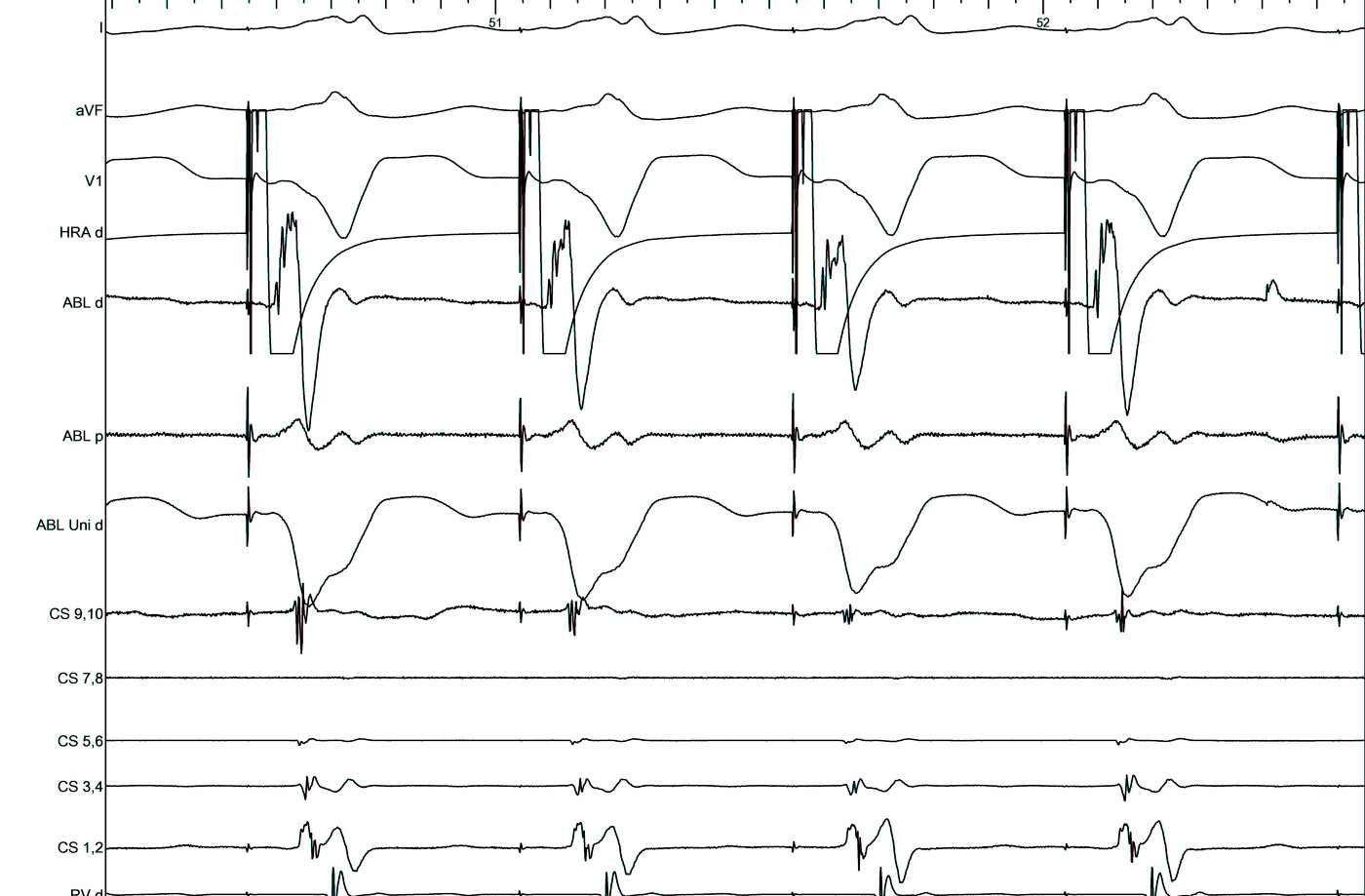
Unipolar EGM

Mapping and ablating in AF
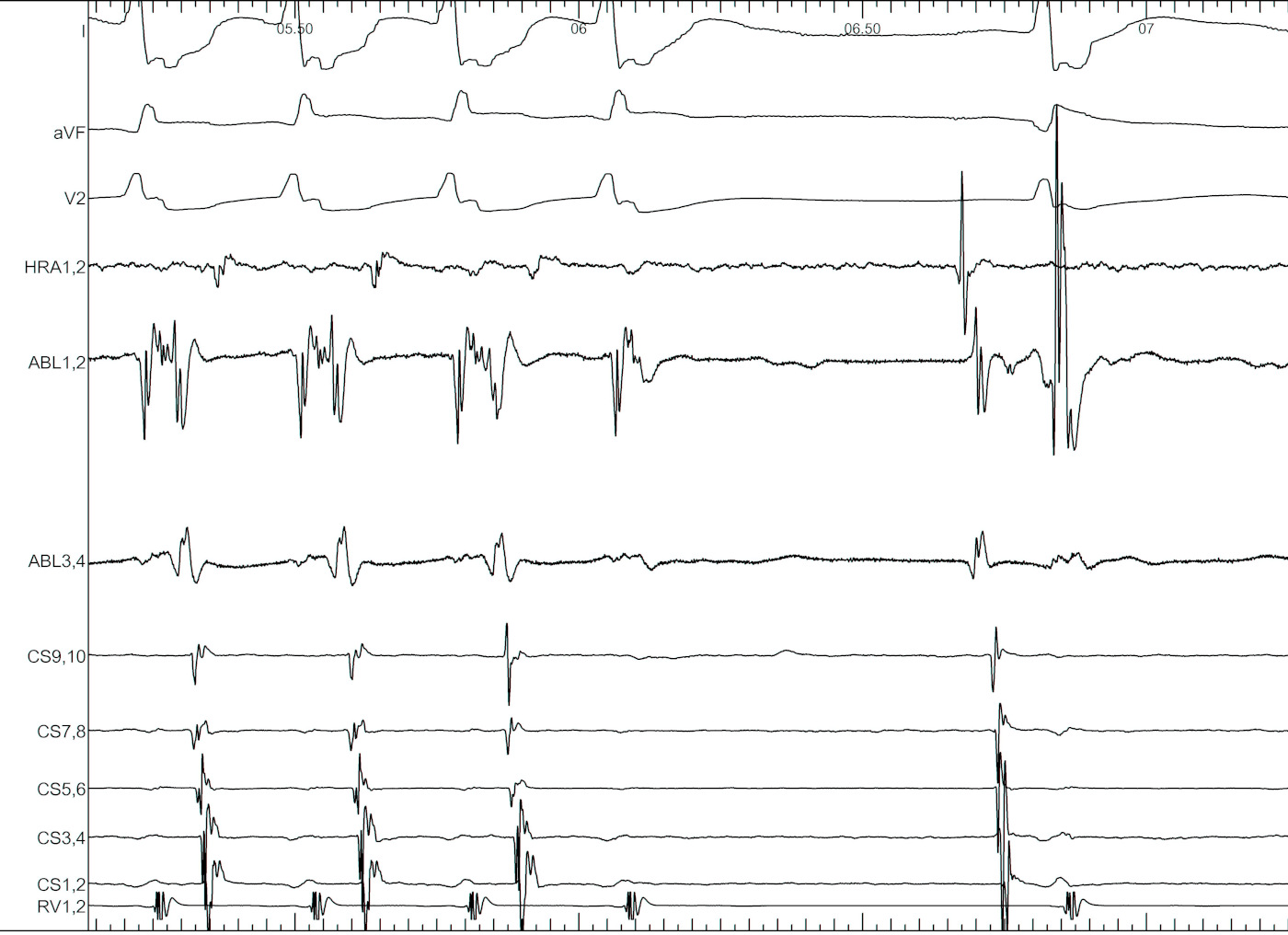
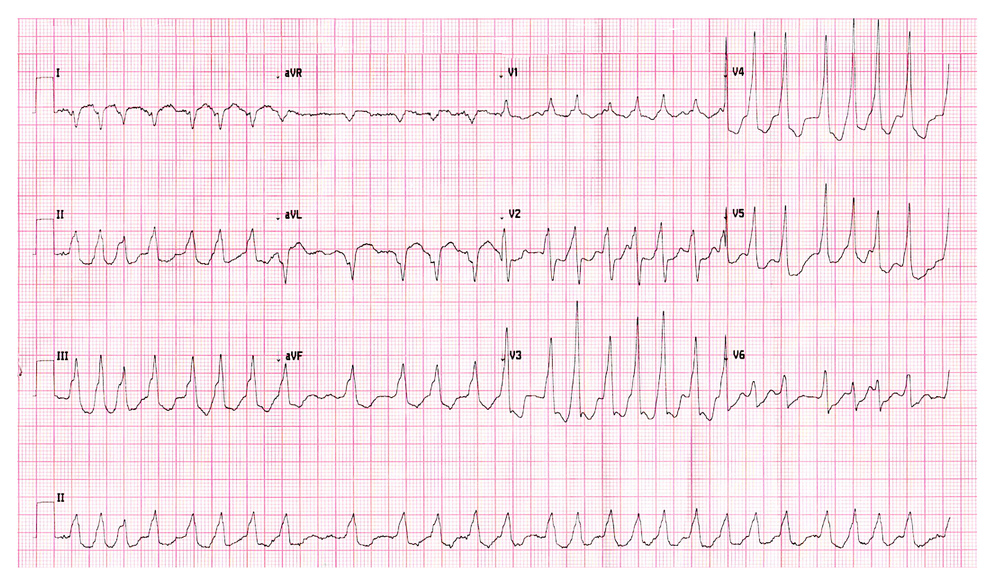
Young male, RHD MS with left sided AP, preexcited AF
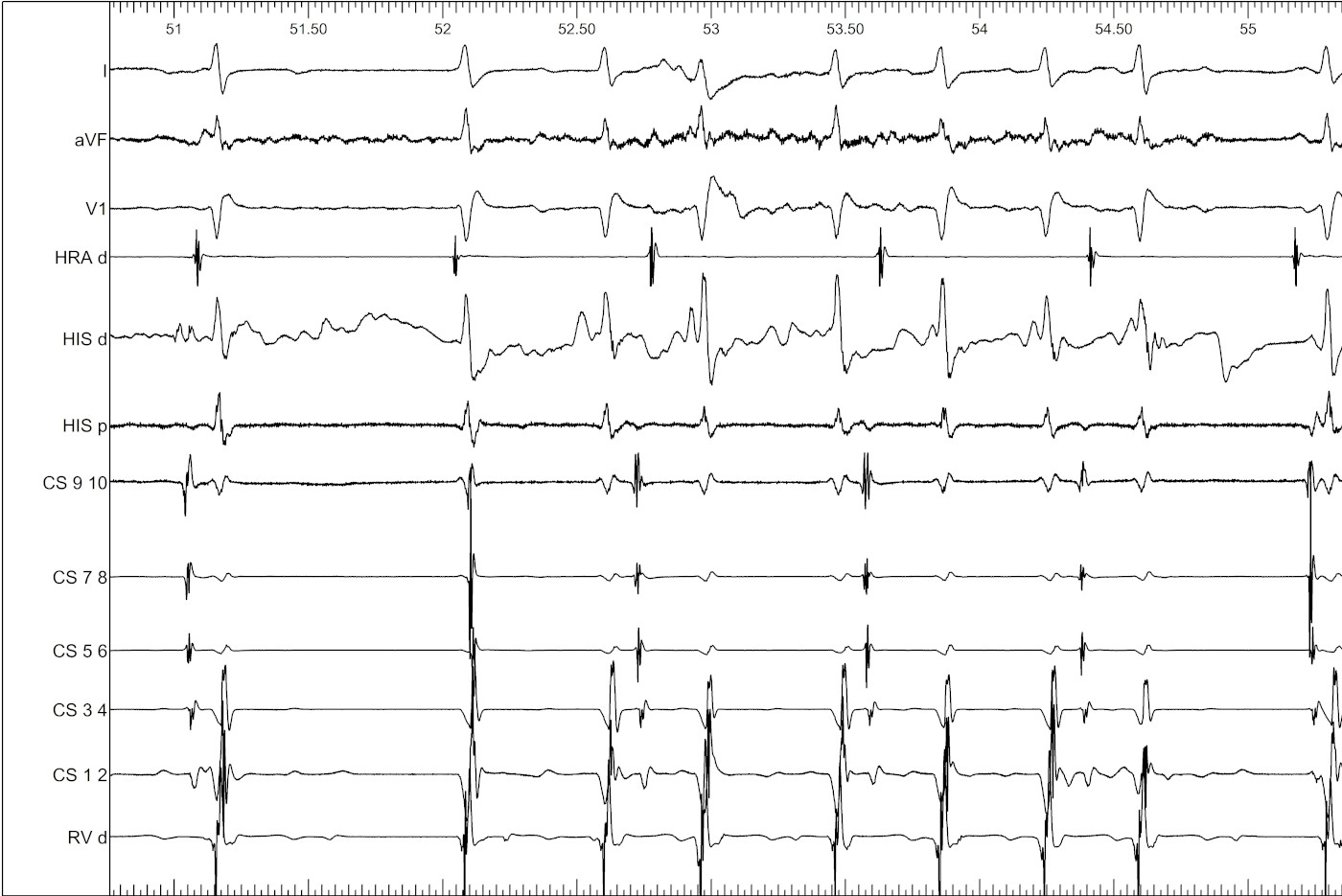
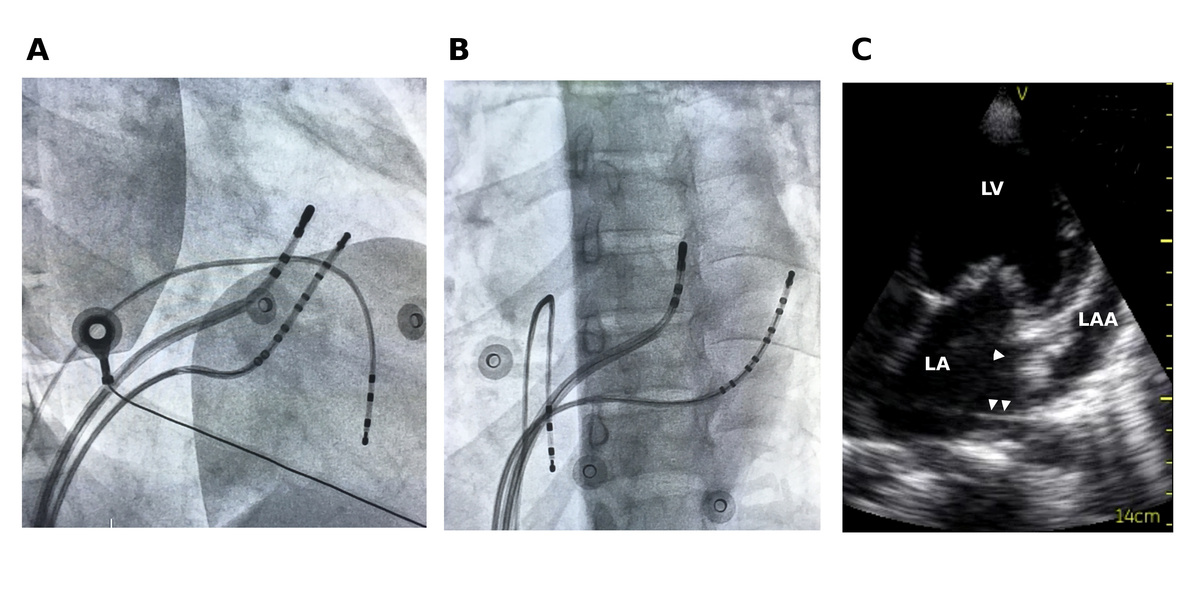
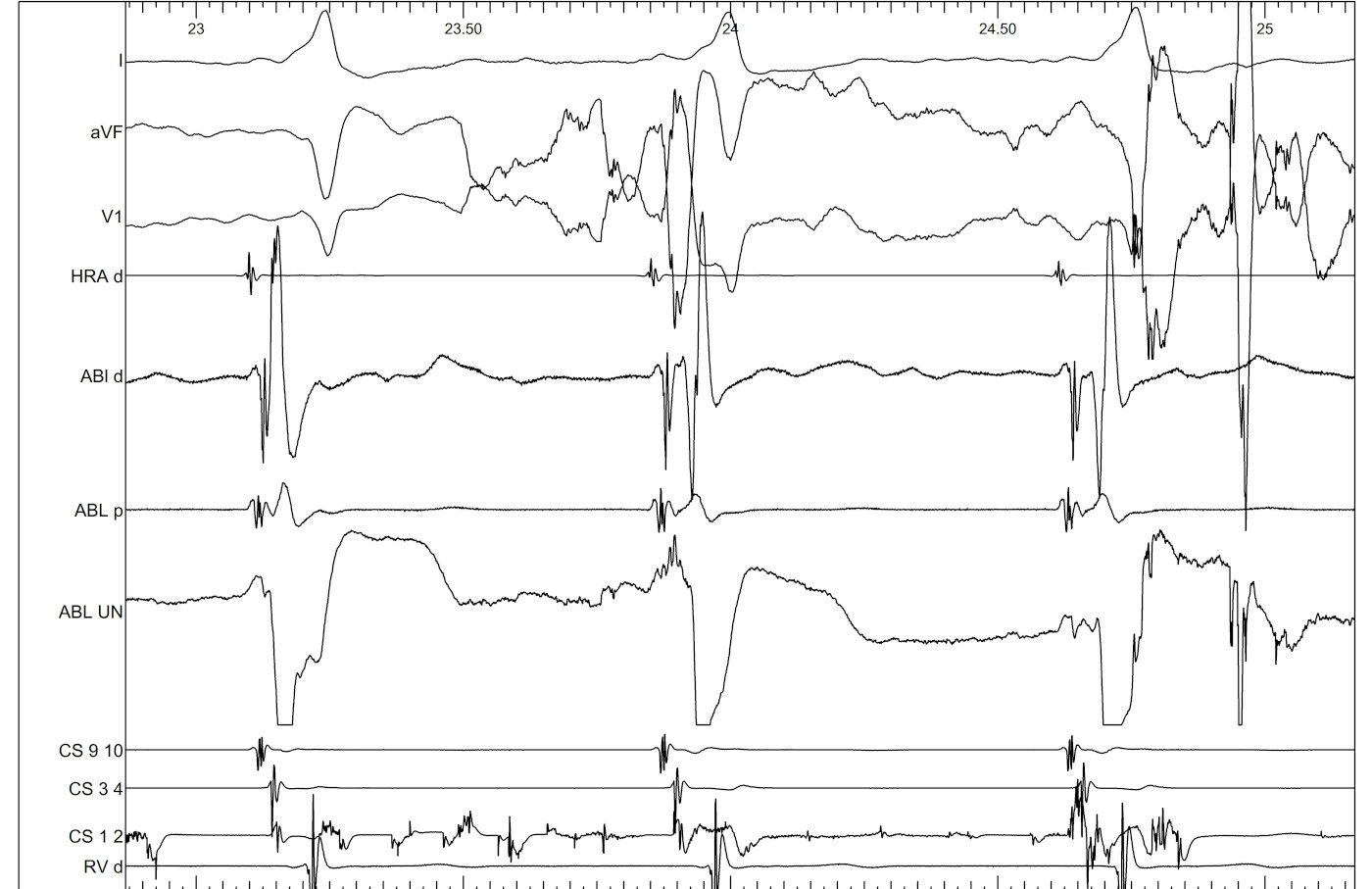
Mapping during AF

Ablation during AF
Using the "bump"


Pathway slant
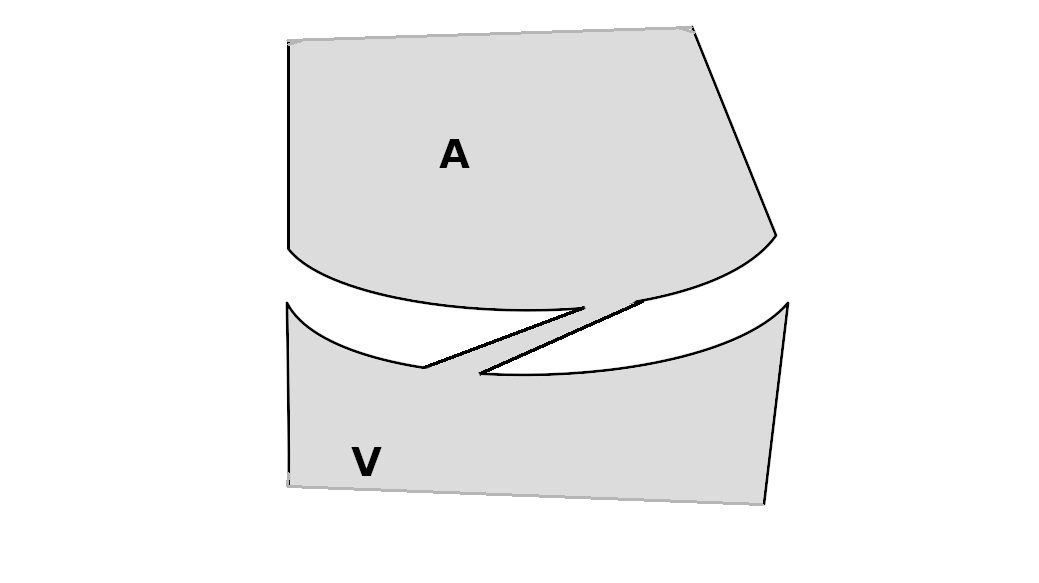
Implications
- Map for earliest A, not shortest VA
- Atrial and ventricular insertions may not correspond
- May be preferable to ablate medial to atrial insertion, where AP potential is observed
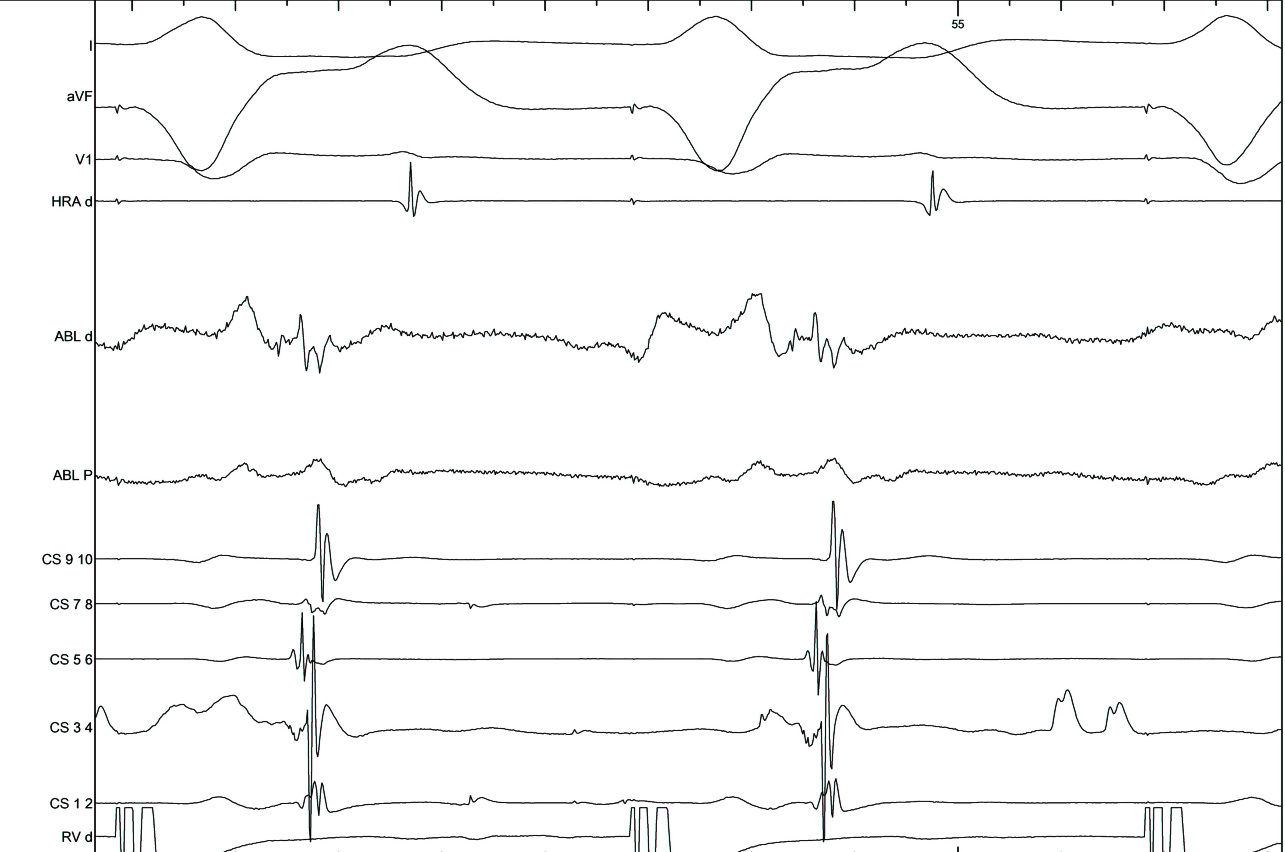
LA - CS potentials
Endocardial AP
Epicardial AP
Unusual locations
Female with left sided AP
A-V separated in CS
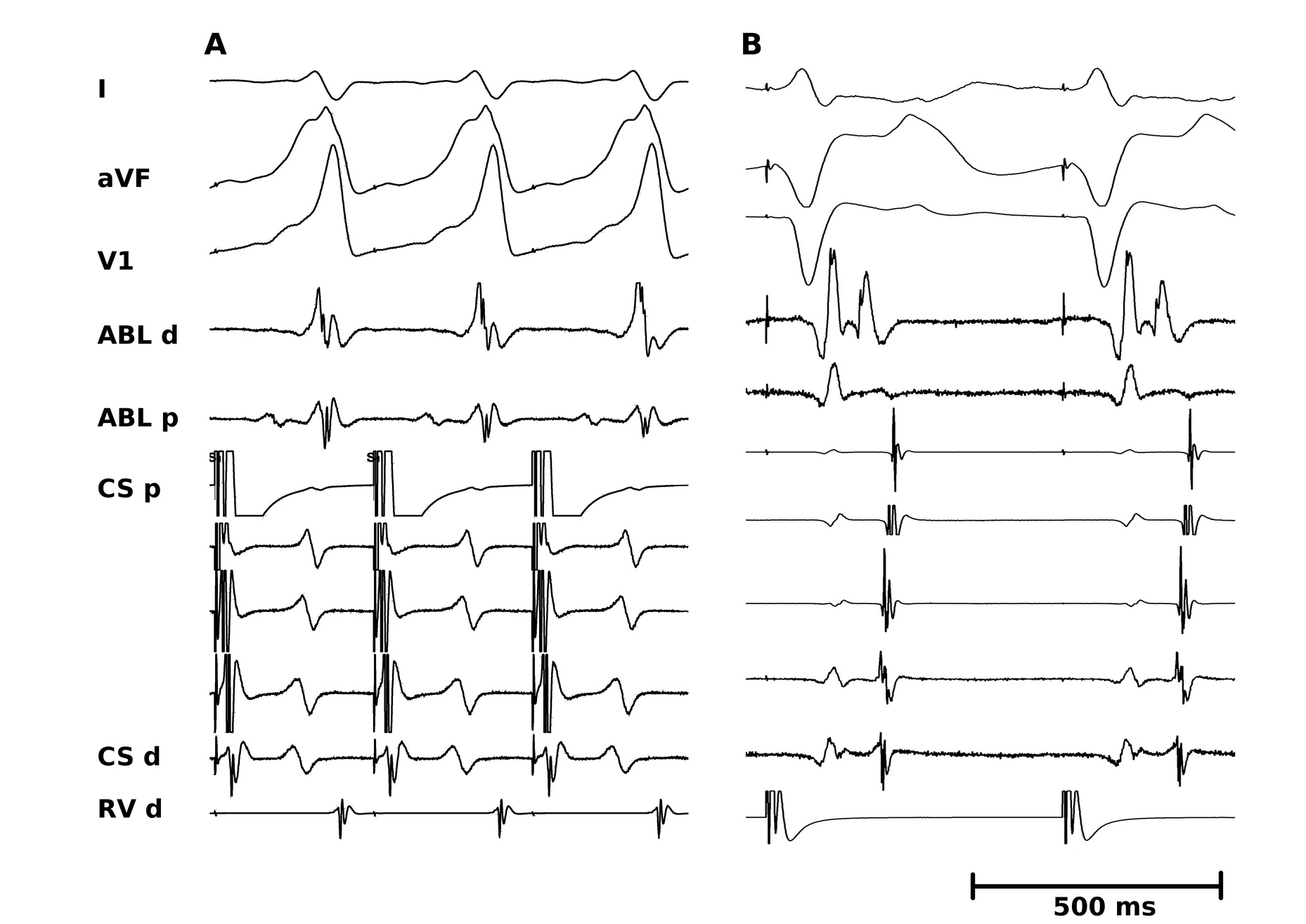
LAA pathway
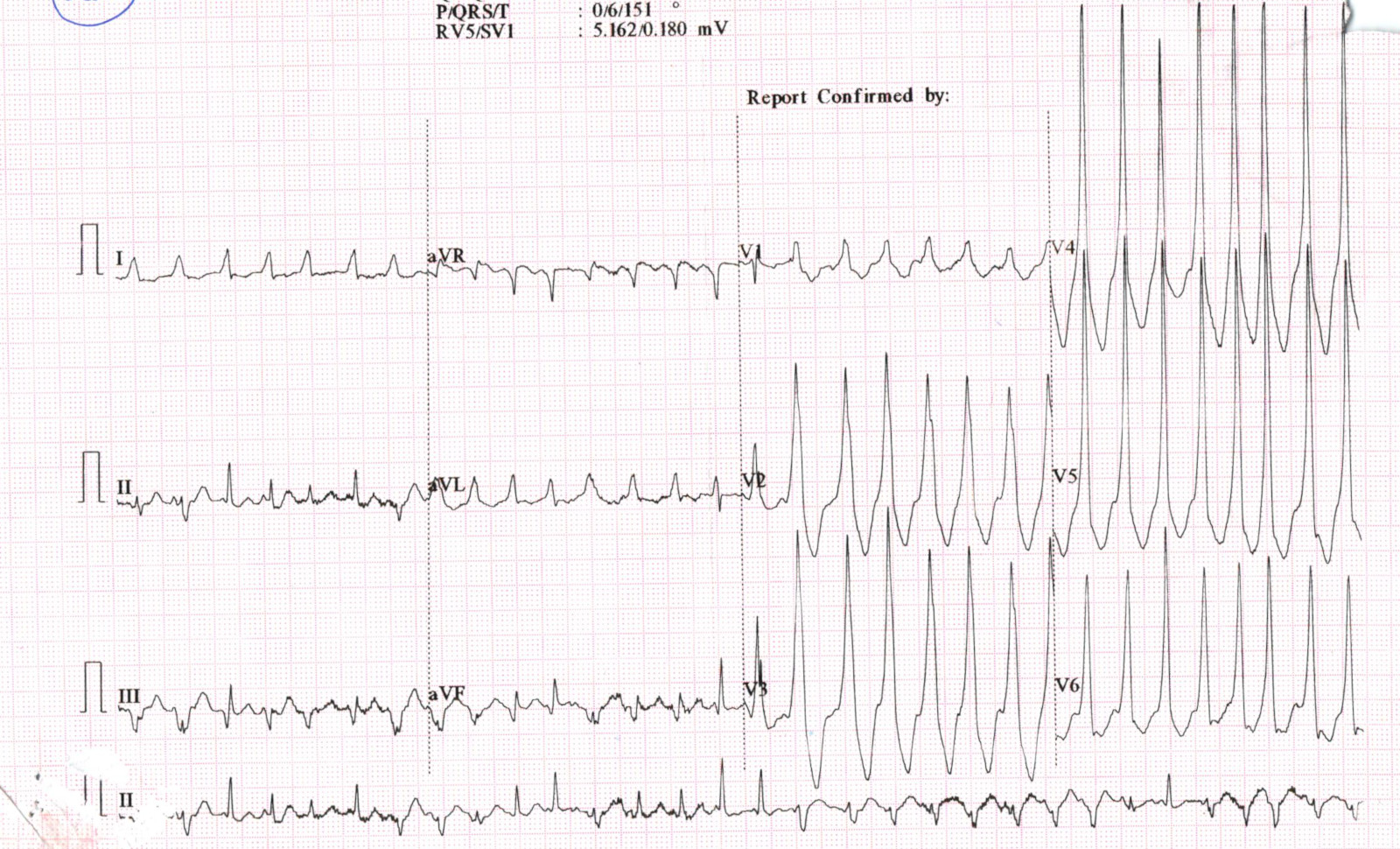
CS Diverticulum
Preexcited AF - note leads II and V6
Venogram
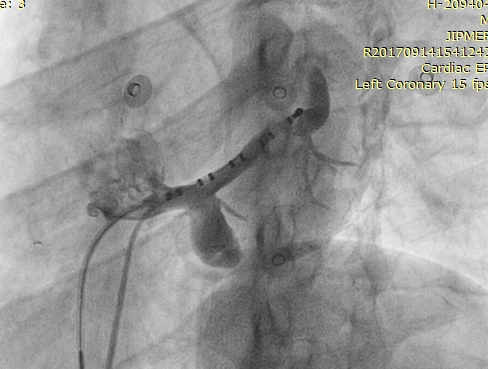
Ablation at ventricular insertion
Successful location at neck with CSE potential

Atrial tachycardia
Activation mapping

Summary
- AVNRT - Ablation within CS / left sided ablation
- AVNRT - VA block in some atypical AVNRT
- AT - Activation mapping. P onset in relation to fixed reference
- AP - Dont ablate when not needed
- AP - Choose rhythm to map and ablate carefully
- AP - When mapping for atrial insertion, map like AT constrained to the annulus
- AP - When mapping the ventricular insertion, Use unipolar EGMs
- Mechanical bump can help to map
- Consider unusual locations - appendages / away from annulus / within CS