Brugada Syndrome - Diagnosis and Management

Raja Selvaraj, JIPMER
What is it
- Inherited disease, first described in 1992
- Autosomal dominant
- Atypical RBBB with ST elevation in right precordial leads
- Malignant arrhythmias
Prevalence and demographics
- Higher incidence in South East Asia, esp Thailand, Philippines and Japan
- About 1:2000 population
- 80% of adult patients are males
- About 20% of sudden death with normal heart
- Triggers - night, large meal, fever
Pathogenesis
- Was initially considered a sodium channelopathy with repolarization abnormalities
- Sodium, Calcium and Potassium channel genetic abnormalities identified
- ? Polygenic
- Repolarization-depolarization abnormalities
- Common phenotypic expression of various abnormalities
Diagnosis
Presentation
- Males, third / fourth decade
- Resuscitated sudden death, syncope, VF
- Typically at night
- Mean age at death around 40 yrs
- Infants and children - symptoms with fever
- Monomorphic VT
ECG findings
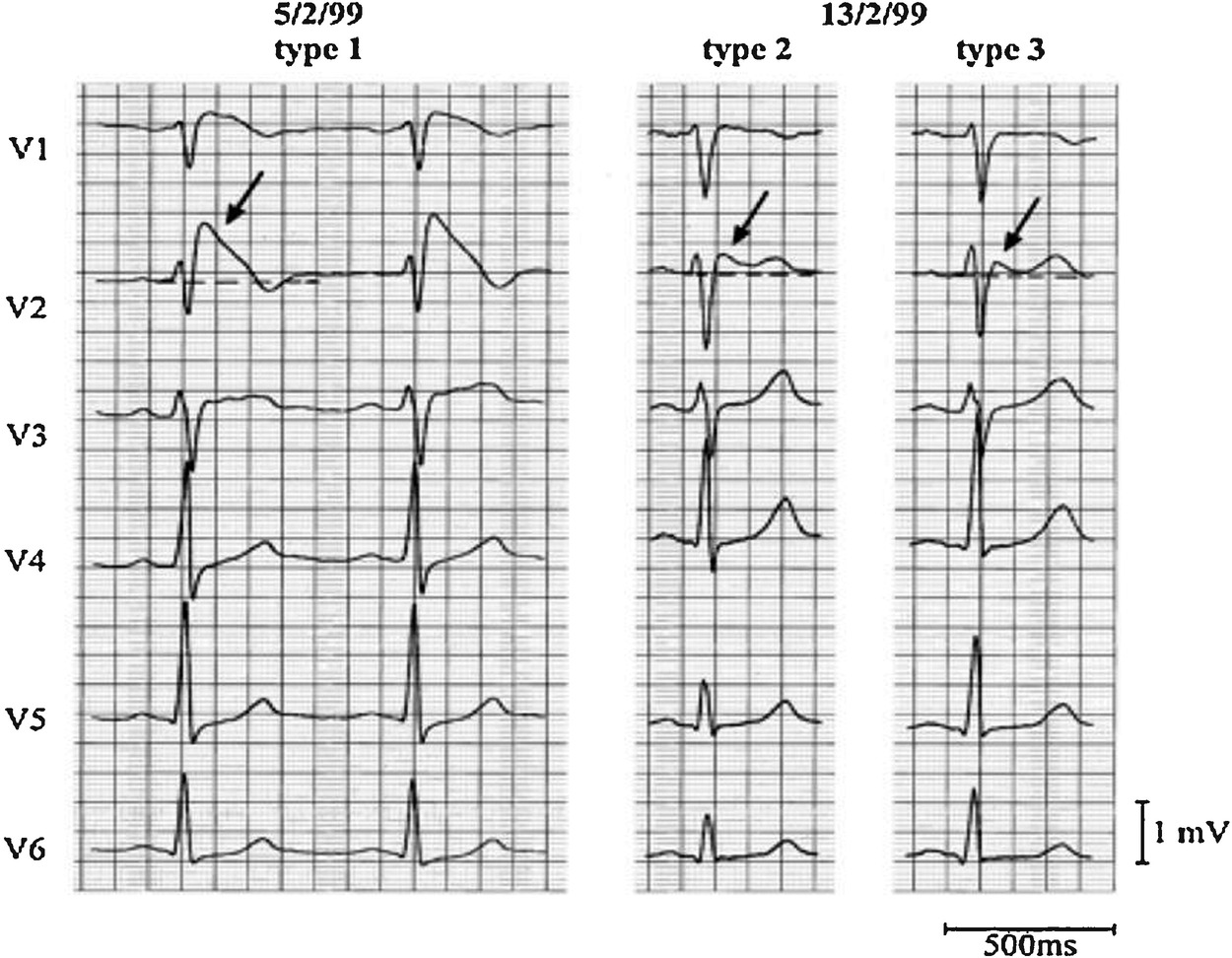
Wilde AA et al. Proposed diagnostic criteria for the Brugada syndrome. Circulation 2002; 106:2514-19
Other ECG findings
- PR prolongation
- Fragmented QRS
- Atrial fibrillation
- Sinus bradycardia / atrial standstill
Diagnostic challenge
- Typical symptoms and type I ECG
- Symptoms, not type I ECG
- No symptoms, type I ECG
Suspicious symptoms, not type I ECG
Drug provocation
- IV Ajmaline - short acting, higher sensitivity
- IV Flecainide
- Oral flecainide (ref)
Drug provocation
- Monitoring
- 3 hrs with Ajmaline
- Longer with flecainide
- Isoprenaline for arrhythmias
- Chest electrodes one space higher
Electrode position
- Electrodes one space higher (V1-V3 in 2nd to 3rd space)
- 12 lead holter with modified V1-V3 and look for changes during nocturnal bradycardia
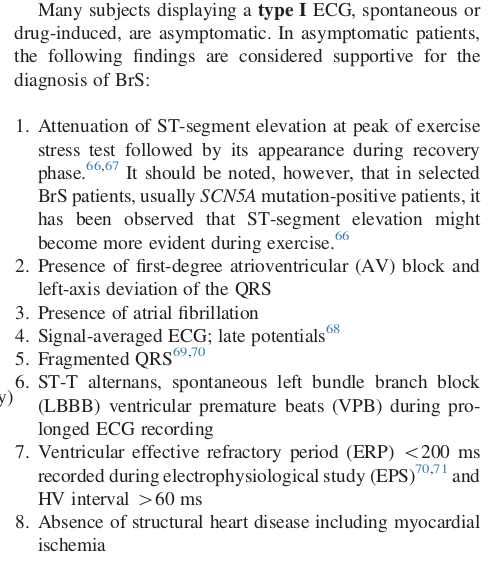
Type I ECG, no symptoms
Misdiagnosis
- Following cardioversion
- Early repolarization
- Athletes heart
- RBBB
- Prinzmetal angina
- Hypothermia
2005 consensus statement - Clinical findings required in addition to ECG
- Documented ventricular fibrillation (VF) / Polymorphic VT
- Family history of sudden cardiac death at <45 years
- Coved-Type ECG in family members
- Inducibility of VT with programmed stimulation
- Syncope or nocturnal agonal respiration (attributed to self-terminating polymorphic VT or VF)
Brugada Syndrome: Report of the Second Consensus Conference. Circulation. 2005;111:659-670
2011 HRS / EPHRA / APHRS consensus
HRS/EHRA/APHRS Expert Consensus Statement on the Diagnosis and Management of Patients with Inherited Primary Arrhythmia Syndromes. Heart Rhythm 2013;10(12):1932-1963
Role of genetic testing
- Generally not considered useful
- Testing for 12 genes equivalent to clinical criteria
Crotti et al. Spectrum and prevalence of mutations involving BrS1- through BrS12-susceptibility genes in a cohort of unrelated patients referred for Brugada syndrome genetic testing: implications for genetic testing J Am Coll Cardiol., 60 (2012), pp. 1410-1418
Outcomes - Annual event rate (1)
- Cardiac arrest - 7.7%
- Syncope - 1.9 %
- Asymptomatic spontaneous type I ECG - 0.5%
Probst et al. Long-term prognosis of patients diagnosed with Brugada syndrome: Results from the FINGER Brugada Syndrome Registry Circulation., 121 (2010), pp. 635-643
Management
Lifestyle measures
- Avoid "Brugada" drugs - brugadadrugs.org
- Prompt treatment of fever
- Avoid excess alcohol
- Avoid big carbohydrate meals at night
Who should get an ICD ?
- Resuscitated cardiac arrest
- Cardiac syncope
Consensus recommendation
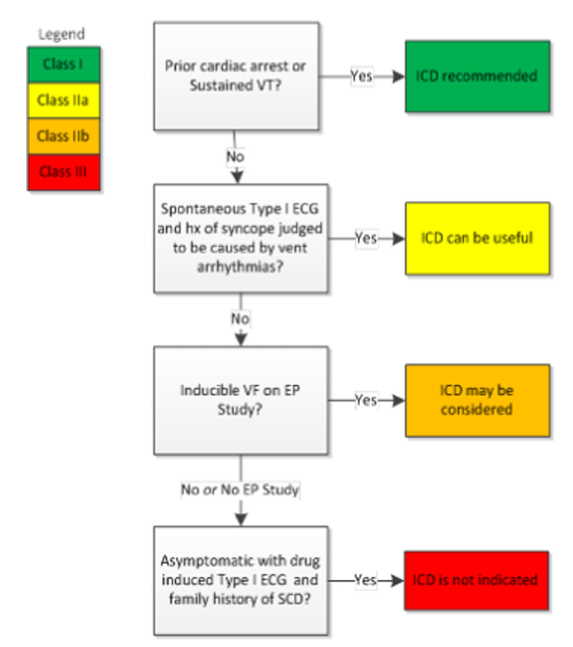
HRS/EHRA/APHRS Expert Consensus Statement on the Diagnosis and Management of Patients with Inherited Primary Arrhythmia Syndromes. Heart Rhythm 2013;10(12):1932-1963
Other risk markers
- Family history of sudden death not an indication
- Spontaneous type I ECG higher risk than provoked type I ECG
- QRS fragmentation, RV ERP < 200 ms, history of syncope, atrial fibrillation
Drugs
- Quinidine effective for long term
- Other drugs - Cilostazol, Tedisamil
- Isoprenaline infusion - for storm
Ablation
- First started with ablation of triggering PVCs
- Abnormal substrate identified in epicardial RVOT and ablated
- Abolition of ECG changes, reduction in clinical episodes
Nademanee K et al. Prevention of ventricular fibrillation episodes in Brugada syndrome by catheter ablation over the anterior right ventricular outflow tract epicardium. Circulation 2011;123:1270–1279
Illustrative case
Presentation
- 45 / Male
- Syncope at home when he woke up and walked to bathroom
- No previous syncope
- Unexplained sudden death in brother
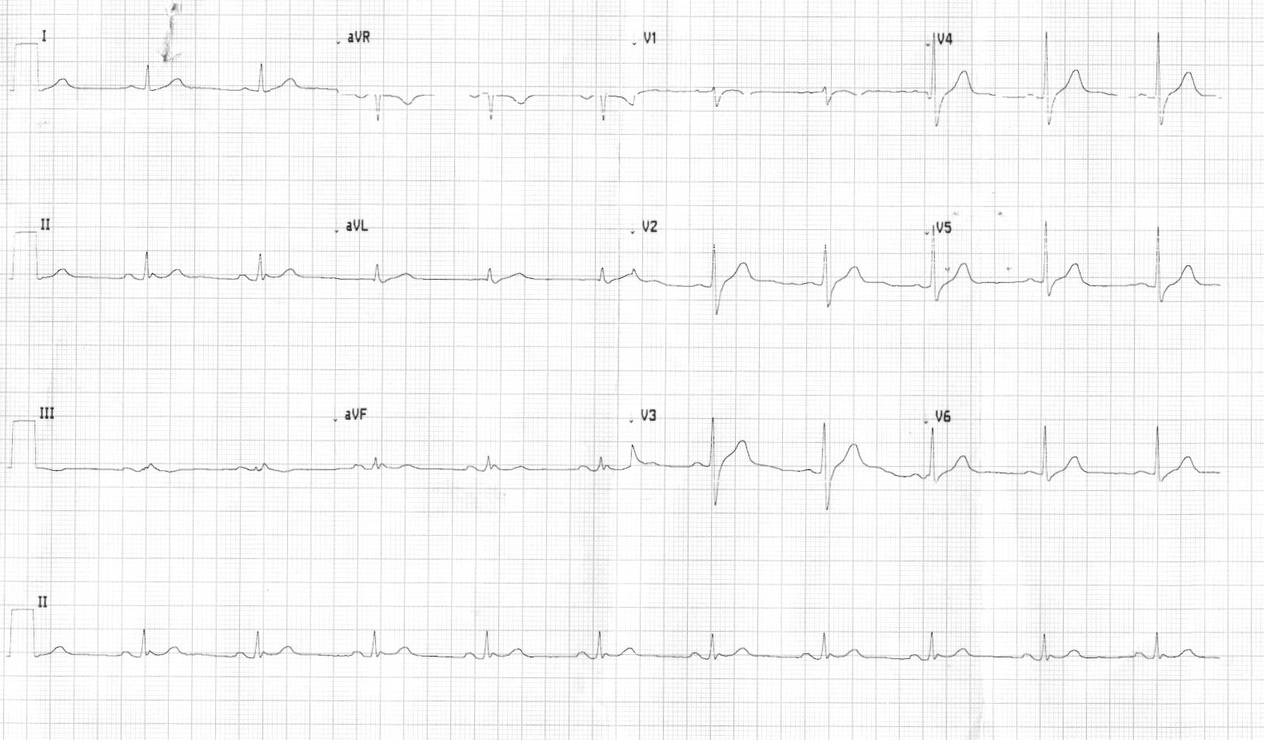
ECG at presentation at local hospital
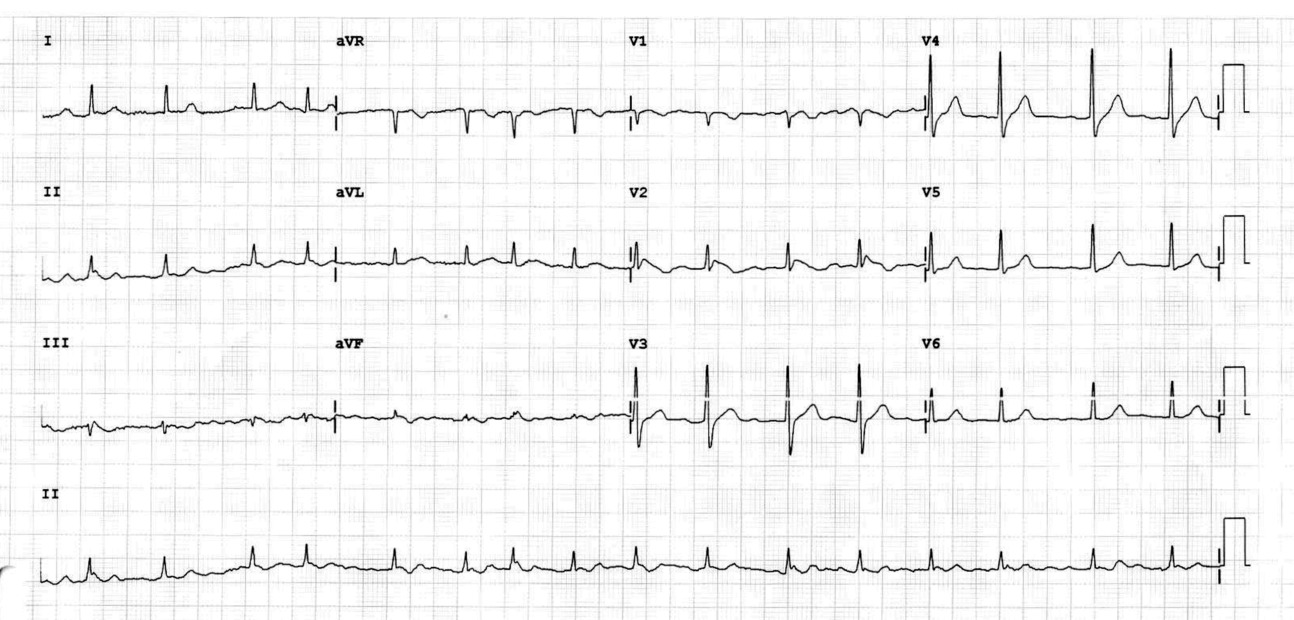
ECG on presentation at JIPMER
Initial diagnosis
- Paroxysmal AF
- Syncope due to AF / Vasovagal
2 hrs post oral flecainide

2 hrs post oral flecainide challenge

- Polymorphic VT - defibrillation, Isoprenaline
- Diagnosed as BrS, AICD implanted
- Recurrent VF with shocks once a month
- no response to Cilostazol
Endo - epicardial mapping
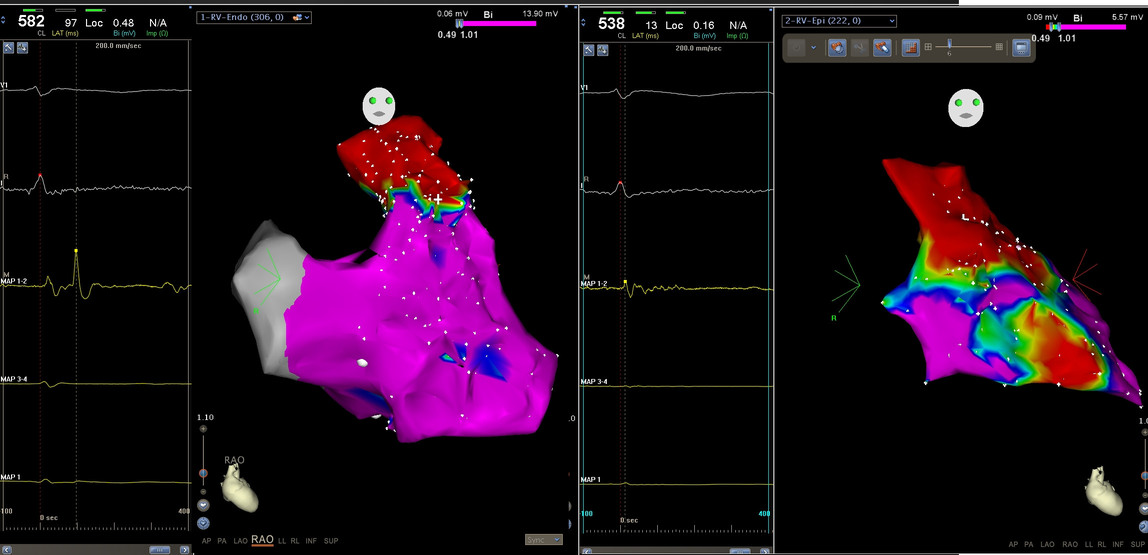
Ablation
- Partial response to ablation
- One episode / yr now, ICD in situ
Summary
- Brugada syndrome is a challenging condition to identify and treat
- Typical symptoms with type I ECG - ICD is indicated
- Look at serial ECGs for subtle signs in patients with symptoms, consider drug provocation, higher position of electrodes
- Asymptomatic type I ECG - only lifestyle changes
- A disease that we are still learning about