Managing the Patient with an AICD

Raja Selvaraj, JIPMER
What information do you need to manage the patient with an AICD?
- What is an AICD ?
- Managing ICD related issues
- How does it affect day-to-day life
- How does it affect medical management ?
What is an AICD
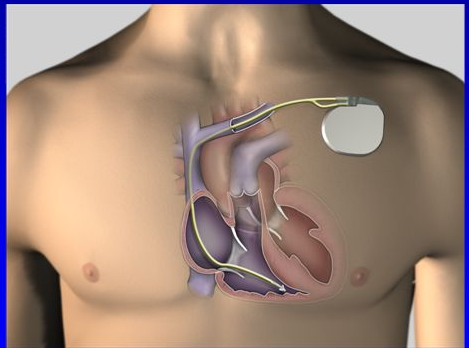
What is an AICD
- A miniaturized battery powered device
- Tracks the heart rate and rhythm
- When there is a tachyarrhythmia, it attempts to correct the rhythm
What does it do?

What it is not
- Does not improve the function of the heart
- Not a treatment for ventricular tachycardia
- Does not prevent tachy-arrhythmias
How does it differentiate an arrhythmia from normal rhythm
- At simplest level, discrimination is rate based
- Other clues are used
- Relation of atrial and ventricular activity
- Morphology of the electrogram
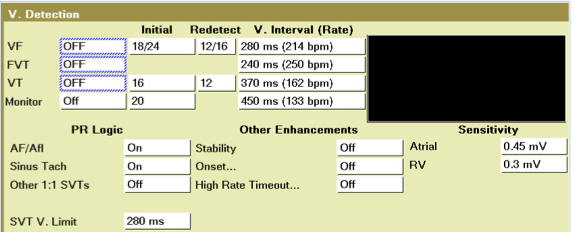
How does it correct the rhythm
- By delivering a biphasic DC shock
- By overdrive pacing
Follow up
- Usually required every 6 months to a year
- Device longevity is generally 5-10 years
- After this needs to be changed (lead retained)
ICD issues
Shock from the device
- Usually felt like a blow on the back / being punched in the chest
- Patient perception varies
- Phantom / inappropriate / appropriate shocks
Need for consultation at specialist center
- One shock + feeling well - early elective device check
- Immediate visit
- More than one shock
- Feeling unwell
Alert from device
- Audible / vibratory alert
- If no other issues, wait one day to confirm alarm (same time each day)
- If repeat alarm, consult at specialist center
Patient who presents with repeated shocks
- Determine if appropriate / inappropriate
- Appropriate - treat arrhythmia
- Inappropriate - may use strong magnet to inhibit therapies
Daily Life
Minimal impact on day to day life
- Diet
- Exercise
- Pregnancy / delivery
- Determined by underlying disease
Driving
- Avoid driving public transport vehicles
- 6 weeks after implantation - Primary prevention
- 6 months without events - Secondary prevention

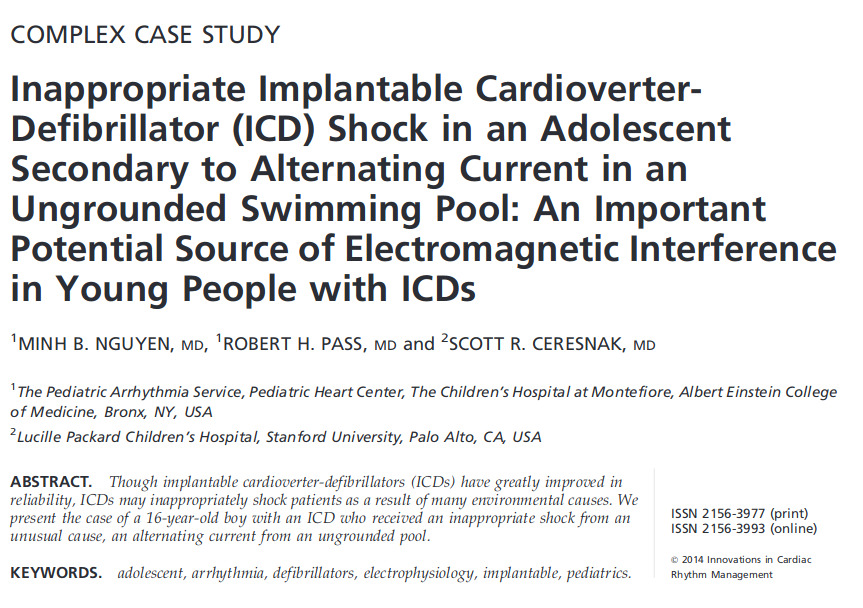
EMI
- No interference from majority of household devices
- Remote control / microwave / electric switches / Walk through scanners at airports
- Mobile phones - 6 inches away - opposite ear / not in shirt pocket
- Music players - headphones 6 inches away
- Anti-theft systems - avoid leaning on / prolonged proximity
- Avoid strong magnets
Suspect EMI
- Shock / symptoms
- Related to place / device
- When in doubt - check in specialist center
Medical management
Drugs
- Most ailments can be treated as usual
- Underlying disease dictates drugs that are safe to use
- Anti-arrhythmic drugs may affect defibrillation threshold
Scans
- CXR / ultrasound - safe
- CT scan - Can sometimes be associated problems when device is directly in scanning field
- MRI - MRI conditional devices - take specialist opinion
Radiotherapy for cancer
- Can damage the device circuitry
- Shield if possible
- Move device if it is in the field
Others
- Extracorporeal shock wave lithotripsy - Avoid
- Transcutaneous electrical nerve stimulation - Avoid on torso, rare interaction when used in limbs
- Electro convulsive therapy - no EMI, but avoid inappropriate therapy for sinus tachycardia
- External defibrillation - keep distance
Surgical procedures
- Cautery can produce EMI
- Bipolar cautery / short bursts / away from device
- Magnet over device / deacivate device
Summary
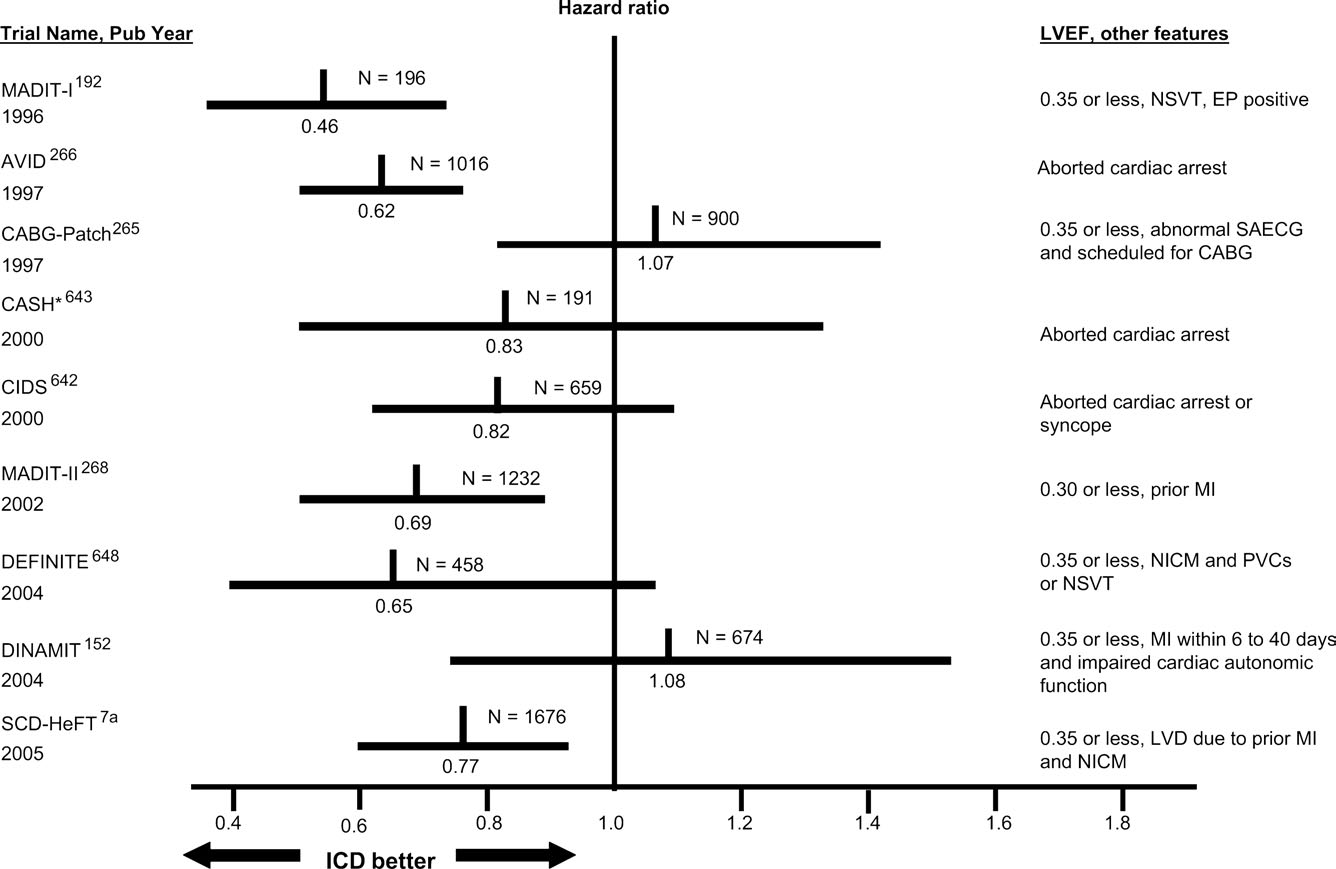
- AICD implants increasing in number
- More such patients will be cared for by cardiologists / physicians
- Many aspects of care related to underlying disease than the ICD
- Understanding of basic aspects of AICD helps manage the patient