CRT - Indications and Response to Therapy

06 April 2019
Raja Selvaraj, JIPMER
Introduction
What is CRT ?
- A third of patients with advanced heart failure have a prolonged QRS duration
- Electrical dyssynchrony associated with mechanical dyssynchrony
- CRT is a form of multisite ventricular pacing that corrects the dyssychrony
- Improvement in systolic function, remodeling of the ventricle, reduction of MR
- Improvement in functional capacity
Illustrative case
- 45 year old male
- DOE NYHA III
- LVEF 18%
- Normal coronaries
CRT implant
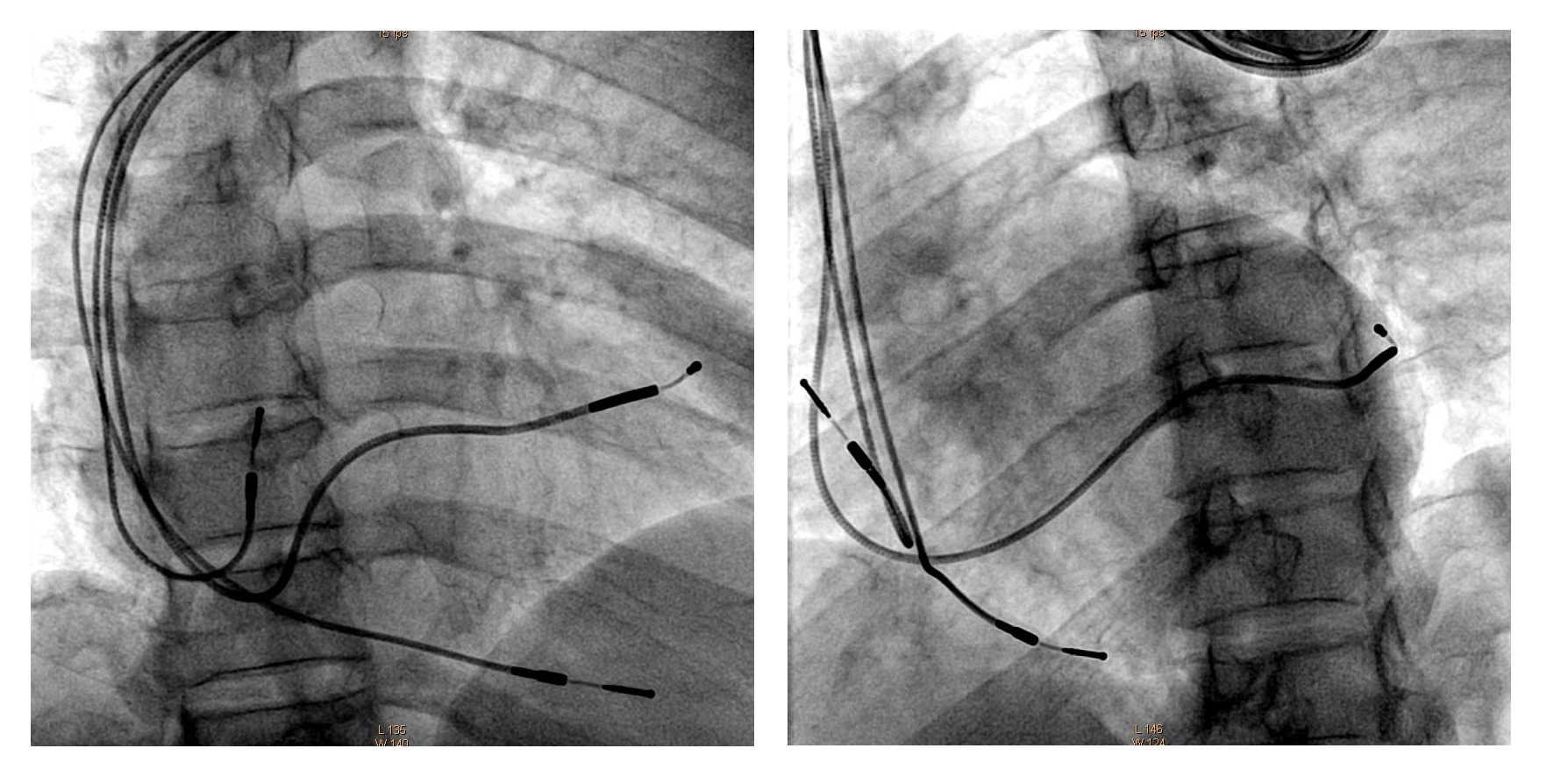
Echo - Pre and Post (3 months)
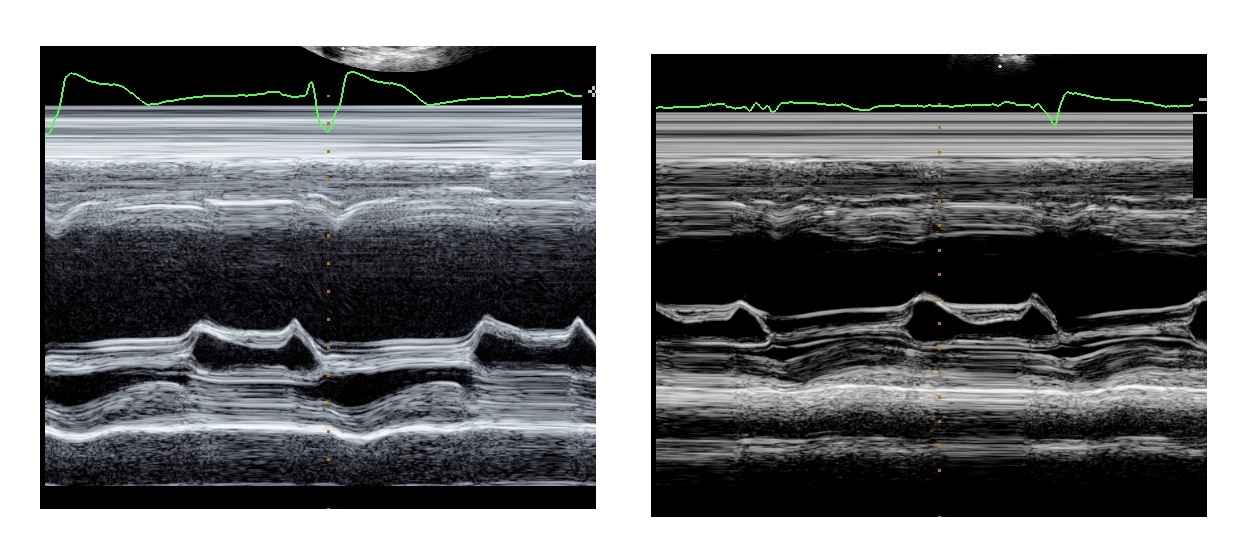
Now - 8 years later
- NYHA I
- LVEF 55%
- Beta blocker and ACEI
Indications
Guidelines based
- ACC AHA guidelines
- Focused update
- EHRA
- ESC
- ACC/AHA/HRS 2008 Guidelines for Device-Based Therapy of Cardiac Rhythm Abnormalities. Circulation. 2008;117:e350–e408
- 2012 ACCF/AHA/HRS focused update incorporated into the ACCF/AHA/HRS 2008 guidelines for device-based therapy of cardiac rhythm abnormalities. J Am Coll Cardiol 62:e6–e75
- 2013 ESC / EHRA guidelines on cardiac pacing and cardiac resynchronization therapy. Eur Heart J 34:2281–2329.
- 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J 18:891–975
Class I Indication
LVEF < 35%
LBBB
QRSd > 150
NYHA II / III / IV
Sinus rhythm
In addition
- Should be receiving guideline directed medical therapy
- Interval more than
- 3 months from initial diagnosis
- 40 days after MI
- 3 months after revascularization
Beyond class I guidelines
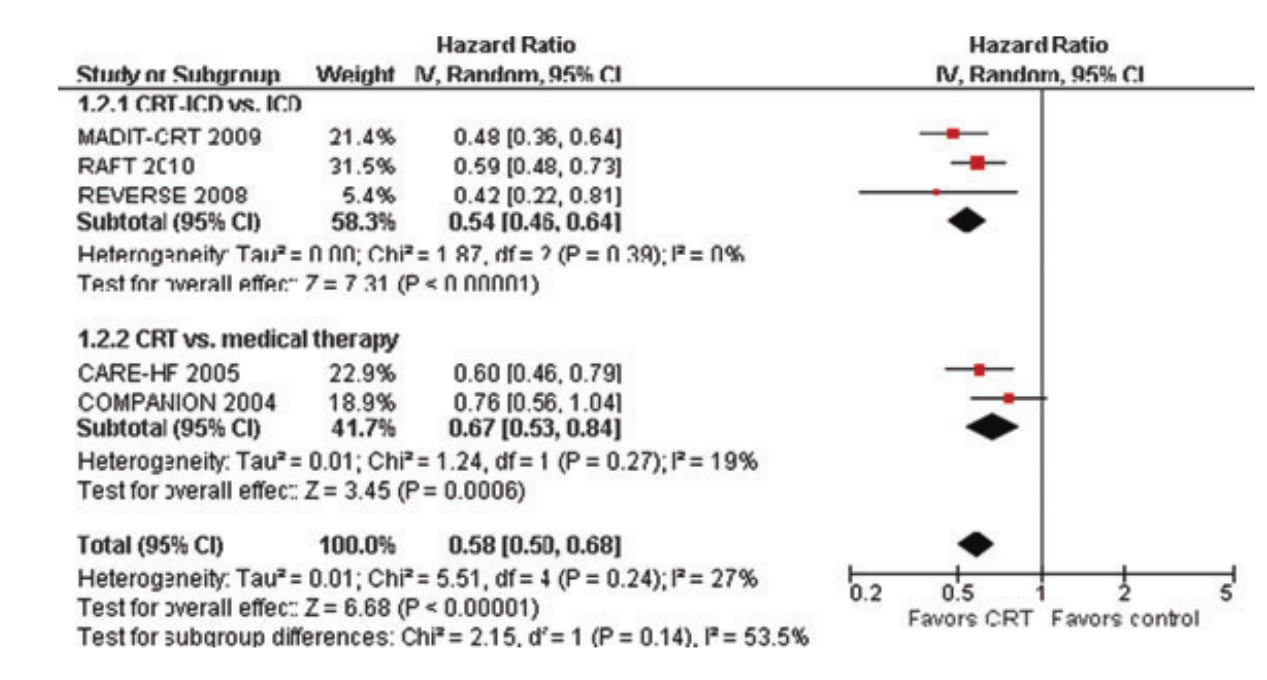
QRS duration < 150 ms
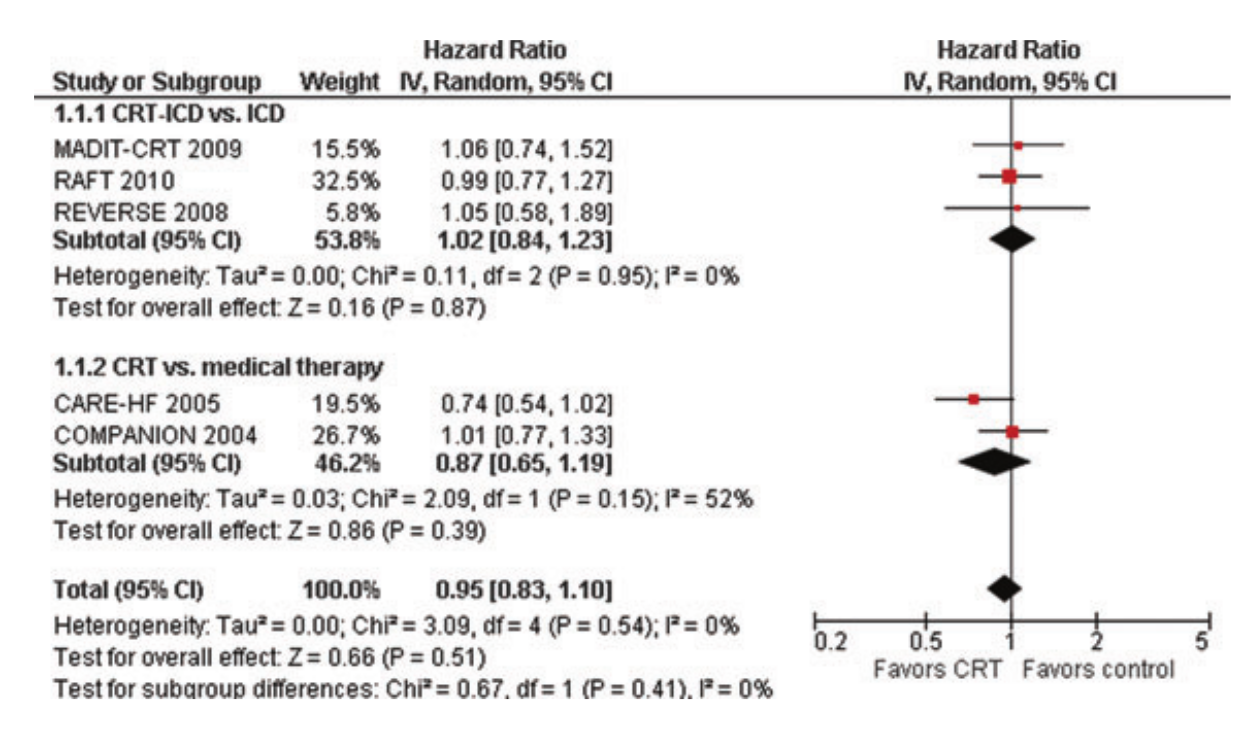
Stavros Stavrakis et al. The Benefit of Cardiac Resynchronization Therapy and QRS Duration: A Meta‐Analysis. JCE 2012;23:163-168
QRS duration < 150 ms
Narrow QRS - QRSd < 120 ms
- Echo identified mechanical dyssynchrony does not predict response
- Class III with QRSd < 120 / 130 ms
- Echo CRT - Ruschitzka F., Abraham W.T., Singh J.P., et al. (2013) Cardiac-resynchronization therapy in heart failure with a narrow QRS complex. N Engl J Med 369:1395–1405
- Lesser earth - Thibault B., Harel F., Ducharme A., et al. (2013) Cardiac resynchronization therapy in patients with heart failure and a QRS complex <120 milliseconds: the Evaluation of Resynchronization Therapy for Heart Failure (LESSER-EARTH) trial. Circulation 127:873–881
QRSd 120-130 ms
- ACC / AHA - Class IIa (2012)
- ESC EHRA - Class I (2013
- ESC HFA - Class III (2016)
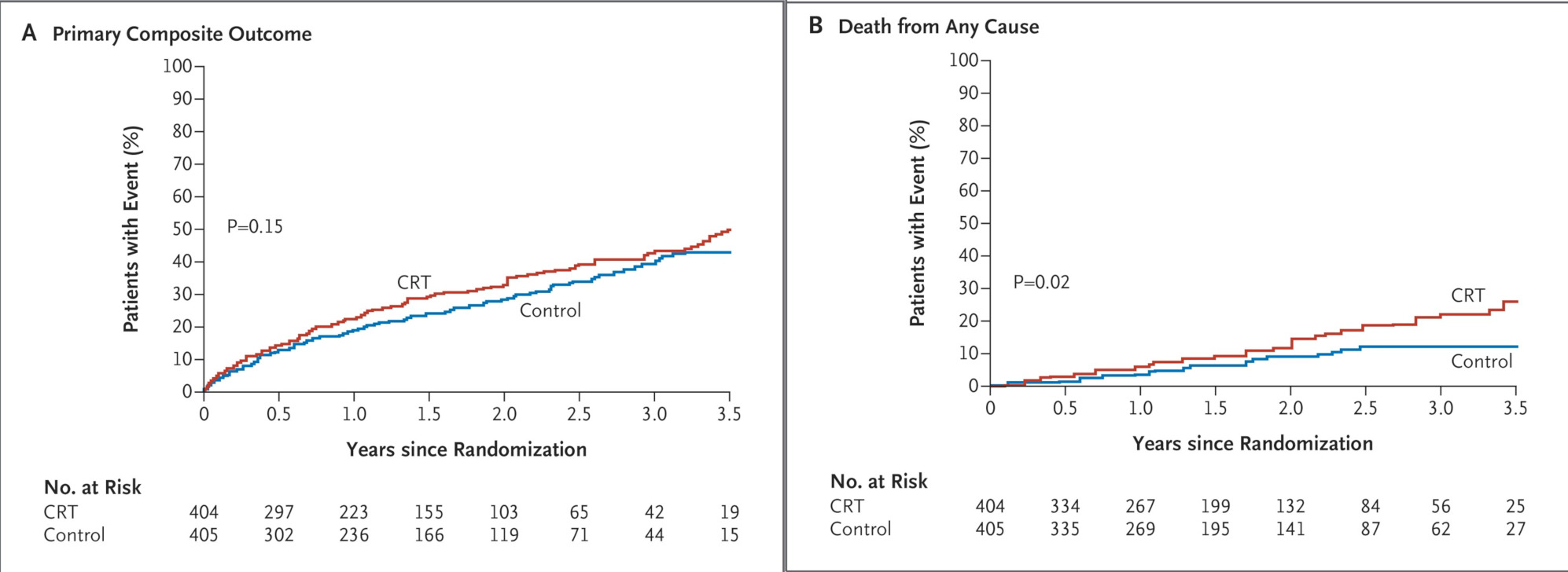
ECHO CRT study
- NYHA III or IV
- LVEF < 35%
- QRSd < 130 ms
- Echo evidence of dyssynchrony
Frank Ruschitzka et al. Cardiac-Resynchronization Therapy in Heart Failure with a Narrow QRS Complex. N Engl J Med 2013; 369:1395-1405
ECHO CRT study
Non LBBB wide QRS
- Class IIa when QRSd > 150 and NYHA III / IV
- Class IIb - NYHA II, QRSd > 150
- Class IIb - NYHA III, QRSd < 150
NYHA Class IV
- Most patients in trials are in NYHA III
- Overall, NYHA IV comprise 10% or less
- Most of these are ambulatory IV
- Not useful in acute decompensated heart failure
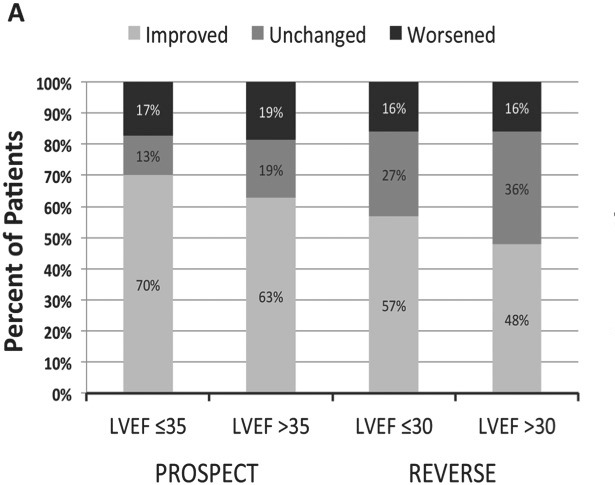
NYHA Class I
- Class IIb indication in ischemic CMP with EF < 30% and LBBB, QRSd>150
- Based on benefit with CRTD in MADIT CRT trial (15% of patients were NYHA I)
Zareba W., Klein H., Cygankiewicz I., et al. (2011) Effectiveness of cardiac resynchronization therapy by QRS morphology in the Multicenter Automatic Defibrillator Implantation Trial-Cardiac Resynchronization Therapy (MADIT-CRT). Circulation 123:1061–1072.
Atrial fibrillation
- Class IIa
- Other indications met
- Ensure near 100% pacing
- Will need good pharmacologic rate control or AV node ablation
Pacing requirement in heart failure or reduced LVEF
- Reduced LVEF
- Heart failure
- Pacing requirement > 40%
- BLOCK HF - Curtis A.B., Worley S.J., Adamson P.B., et al. (2013) Biventricular pacing for atrioventricular block and systolic dysfunction. N Engl J Med 368:1585–1593
- DAVID - Sharma A.D., Rizo-Patron C., Hallstrom A.P., et al. (2005) Percent right ventricular pacing predicts outcomes in the DAVID trial. Heart Rhythm 2:830–834.
Ischemic heart disease
- Not differentiated in guidelines
- Clinical / remodeling response less compared to NICM
- Survival benefit of CRTD over ICD in trials
- Predominantly used in North America (>50% of all CRT)
Heart failure, LBBB, EF 35-50%
Evolution of CRT usage
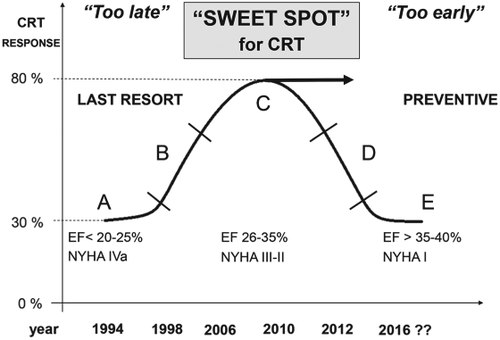
Summary
Summary
- Better selection = less non responders
- Situations where trial may be considered although chance of response less
- Should be discussed with patient